Use of High dose Corticosteroids Reversed COVID-19 Associated ARDS in a Patient Listed for Lung Transplantation
JM Kwakkel-van Erp1,2*, K Dams3, V Verplancke1, P Raman1, D Ruttens4,5, SE Thiessen6, I Baar3, R Jacobs3, P Lauwers7, K Yogeswaran7, SE Verleden1,2,7, JMH Hendriks2,7
1Department of Pulmonology, University Hospital Antwerp, Antwerp, Belgium
2University of Antwerp, Antwerp, Belgium
3Department of Intensive Care, University Hospital Antwerp, Antwerp, Belgium
4Department of Pulmonology, ZOL (Hospital of East Limburg), Genk, Belgium
5Department of Medicine and Life Sciences, Hasselt University, Diepenbeek, Belgium
6Department of Intensive Care, ZOL (Hospital of East Limburg), Genk, Belgium
7Department of Thoracic and Vascular Surgery, University Hospital Antwerp, Belgium
*Corresponding Author: Hanneke JM Kwakkel-van Erp, Department of Pulmonology, University Hospital Antwerp, Antwerp, Belgium
Received: 27 March 2022; Accepted: 13 April 2022; Published: 22 April 2022
Article Information
Citation: JM Kwakkel-van Erp, K Dams, V Verplancke, P Raman, D Ruttens, SE Thiessen, I Baar, R Jacobs, P Lauwers, K Yogeswaran, SE Verleden, JMH Hendriks. Use of High dose Corticosteroids Reversed COVID-19 Associated ARDS in a Patient Listed for Lung Transplantation. Archives of Clinical and Medical Case Reports 6 (2022): 281-285.
View / Download Pdf Share at FacebookAbstract
Patients with COVID-19 associated ARDS have a mortality rate varying from 30-60%. If there is mono-organ failure and recovery is deemed unlikely despite optimal care, these patients are eligible for lung transplantation. We present our experience with high dose corticosteroid pulse therapy in an ICU patient on ECMO and mechanical ventilation, listed for lung transplantation. The patient responded with improved oxygenation, was weaned from ECMO and delisted from lung transplant waiting list.
Keywords
<p>COVID-19, Lung Transplantation, Acute Respiratory Distress Syndrome</p>
Article Details
1. Introduction
Lung transplantation is an accepted treatment for end-stage lung diseases. In Acute Respiratory Distress Syndrome (ARDS) patients with irreversible lung damage, lung transplantation from a ventilator and/or Extracorporeal Membrane Oxygenation Support (ECMO) is feasible and accepted in some cases [1]. Patients with COVID-19 associated ARDS have a mortality rate varying between 30-60% [2-5]. Selection criteria for potential lung transplant candidates with a COVID-19 associated ARDS have been published [6]. One of the selection criteria for COVID-19 associated ARDS is the presence of irreversible lung damage and subsequently implicates that recovery is regarded unlikely despite optimal care (including mechanical ventilation and/or ECMO support) [6]. Well selected patients transplanted for COVID-19 associated ARDS, have good outcomes [7]. We present our experience with high dose corticosteroid treatment in a patient with COVID-19 associated ARDS, listed for bilateral lung transplantation, who could be weaned from ECMO and ventilation and is no longer oxygen dependent [6].
2. Case Report
A 50-year-old female non-smoker, BMI of 29.6, with a medical history of Multiple Sclerosis (relapsing-remitting type under treatment with anti-alpha4 -integrin therapy) and stable monoclonal gammopathy of undetermined significance, was tested positive for COVID-19. Six days later, she deteriorated and was admitted to the hospital. High flow oxygen and dexamethasone (six milligram daily), were started and for two weeks patients remained stable. Unfortunately, 20 days after testing positive for COVID-19), patient was admitted to the Intensive Care Unit (ICU) and developed a severe ARDS with need for mechanical ventilation and ECMO support. Corticosteroids according to the Meduri scheme and ciprofloxacin were started [8]. Weaning trials were initiated but failed and CT-thorax showed consolidation and presumed fibrosis (see Figure 1). To manage fluid overload, continuous veno-venous hemofiltration was started and another trial with corticosteroids according to the Meduri scheme was initiated. After 37 days on ECMO, she was transferred to our hospital for evaluation for lung transplantation. Patient was listed for bilateral lung transplantation after multidisciplinary consensus. A corticosteroid pulse therapy of 1000 mg of methylprednisolone IV for three days during antibiotic coverage with piperacillin/tazobactam was started and within three days the clinical condition of the patient improved so that she could be weaned from ECMO (51 days of ECMO) and delisted from the lung transplantation waiting list. Due to immobilization, she had developed critical illness neuropathy and a Ventilator-Associated Pneumonia (VAP) with a Klebsiella pneumoniae that was complicated by an ARDS and passagère kidney failure with a need for continuous veno-venous hemofiltration (12 days of CVVH). Eventually, patient recovered and could be successfully weaned from the ventilator (total ventilation time of 67 days). Now 9 months after her COVID-19 infection, patient does not require oxygen, is walking with a stick and has an improving lung function (see Table 1).
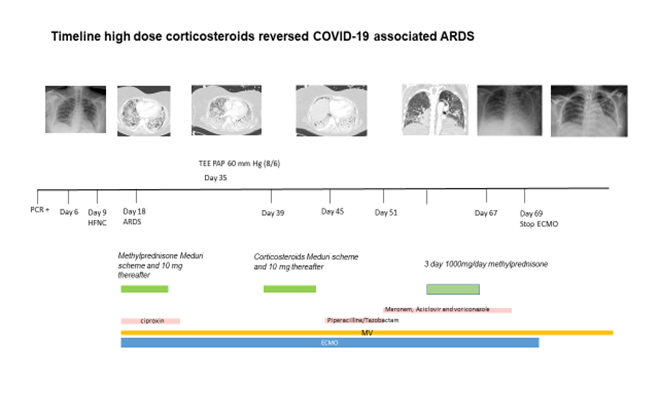
Figure 1: Timeline depicting treatment throughout hospitalization.
PCR = polymerase chain reaction, HFNC = high flow oxygen with nasale canule, MV = mechanical ventilation, ECMO = extracorporeal membrane oxygenation.
|
unit |
Predicted |
7 months after COVID infection |
4 months after COVID infection |
|
|
FVC (%) |
L |
3.31 |
2.26 (68.5%) |
2.08 (62.9%) |
|
FEV1 |
L |
2.65 |
1.93 (73.0%) |
1.79 (67.6%) |
|
FEV1/FVC |
% |
85 |
86 |
|
|
PEF |
L/S |
6.19 |
5.50 (89.2%) |
5.10 (82.4%) |
|
RV |
L |
1.7 |
1.22 (71.1%) |
1.15 (67.7%) |
|
TLC |
L |
4.77 |
3.64 (76.2%) |
3.23 (67.7%) |
|
DLCO |
mmol/(min*kPa) |
6.79 |
3.33 (49%) |
|
|
DLCO/ VA |
mmol/(min*kPa) |
1.46 |
1.19 (81.5%) |
|
|
VA |
L |
4.68 |
2.79 (59.6%) |
|
|
FVC = Forced vital capacity, FEV1 = Forced expiratory volume in 1 second, PEF = peak expiratory flow, RV = Residual volume, TLC = Total lung capacity, DLCO = diffusing capacity for carbon monoxide, VA = alveolar volume |
||||
Table 1: Spirometry after high dose pulse corticosteroids.
3. Discussion
COVID-19 associated ARDS has a high mortality rate and in a minority of these patients lung transplantation is feasible. Corticosteroid treatment according to the Meduri scheme is an acknowledged therapy in COVID-19 associated ARDS. Here, we report the efficacy of a regimen with high dose corticosteroids as ultimate salvage therapy, despite Meduri scheme attempts, in a patient that was listed for transplantation.
Corticosteroids are beneficial for immunomodulation and may reduce hyperinflammation. Although there are no trials whether the use of pulse dose is beneficial or not, there exist some clues: limited number of cases in COVID-19 encephalopathy and non-intubated and intubated COVID-19 patients [9-11]. Post-mortem studies of COVID-19 infected patients reported diffuse alveolar damage with perivascular and interstitial mononuclear cell infiltration, multifocal endothelitis and COVID-19 induced vasculitis [12, 13]. Following lung transplantation, the phenomenon of interstitial and perivascular mononuclear cell infiltration is also a known complication, seen in acute rejection and treated with high dose corticosteroids (1000 mg methylprednisolone IV for three days). In line with this phenomenon, the beneficial effect of high dose pulse corticosteroids in COVID-19 encephalopathy, and stimulated by the facts that COVID-19 associated vasculitis has been acknowledged and that in COVID-19 a radiological pattern compatible with organizing pneumonia is observed which is treated with high dose corticosteroids, we treated our patient with high dose corticosteroids (1000 mg methylprednisolone IV for three days).
Our trial with administration of high dose corticosteroids pulse therapy (1000 mg once a day, for three days) in COVID-19 ARDS patients refractory to corticosteroids according to “classical schemes” has been successful and is informative. This patient responded to the high dose corticosteroid pulse therapy with improved oxygenation, which in our opinion led to her clinical improvement. Eventually she was delisted from the lung transplantation waiting list. In a retrospective single center study, a three-day rescue course of 1000 mg/day of methylprednisone i.v. was administrated within the first 10 days of treatment showed a response, defined as any improvement in the PaO2/FiO2 ratio over the first week after the bolus in more than 50% of these patients [14]. Unfortunately, they were not able to identify factors associated with this response. Further studies, some of which are on the way, will hopefully further elucidate responders and non-responders to high dose corticosteroid pulse therapy and preferably answer the question if prophylactic use of antibiotics and antifungals (in view of possible complications such as pulmonary aspergillosis and mucormycosis) is prudent in this vulnerable group.
References
- Chang Y, Lee SO, Shim TS, et al. Lung Transplantation as a Therapeutic Option in Acute Respiratory Distress Syndrome. Transplantation 102 (2018): 829-837.
- Li Bassi G, Suen JY, Dalton HJ, et al. An appraisal of respiratory system compliance in mechanically ventilated covid-19 patients. Critical care (London, England) 25 (2021):199.
- Barbaro RP, MacLaren G, Boonstra PS, et al. Extracorporeal membrane oxygenation support in COVID-19: an international cohort study of the Extracorporeal Life Support Organization registry. Lancet 396 (2020): 1071-1078.
- Estenssoro E, Loudet CI, Ríos FG, et al. Clinical characteristics and outcomes of invasively ventilated patients with COVID-19 in Argentina (SATICOVID): a prospective, multicentre cohort study. The Lancet Respiratory medicine 9 (2021): 989-998.
- Dmytriw AA, Chibbar R, Chen PPY, et al. Outcomes of acute respiratory distress syndrome in COVID-19 patients compared to the general population: a systematic review and meta-analysis. Expert review of respiratory medicine 15 (2021): 1-8.
- Bharat A, Machuca TN, Querrey M, et al. Early outcomes after lung transplantation for severe COVID-19: a series of the first consecutive cases from four countries. The Lancet Respiratory medicine 9 (2021): 487-497.
- Roach A, Chikwe J, Catarino P, et al. Lung Transplantation for Covid-19-Related Respiratory Failure in the United States. N Engl J Med 386 (2022): 1187-1188.
- Meduri GU, Bridges L, Shih MC, et al. Prolonged glucocorticoid treatment is associated with improved ARDS outcomes: analysis of individual patients' data from four randomized trials and trial-level meta-analysis of the updated literature. Intensive Care Med 42 (2016): 829-840.
- Montaut V, Madigan S, Pugin D, et al. Corticosteroid Responsive Encephalopathy: Prolonged Coma in Patients Late in the Course of Dreadful Severe Acute Respiratory Syndrome Coronavirus 2 Infection. Critical care explorations 2 (2020): e0248.
- Gunawardhana C, Nanayakkara G, Gamage D, et al. Delayed presentation of postinfectious encephalitis associated with SARS-CoV-2 infection: a case report. Neurological sciences: official journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology 42 (2021): 3527-3530.
- Callejas Rubio JL, Luna Del Castillo JD, de la Hera Fernández J, et al. Effectiveness of corticoid pulses in patients with cytokine storm syndrome induced by SARS-CoV-2 infection. Medicina clinica (English ed) 155 (2020): 159-161.
- Ackermann M, Verleden SE, Kuehnel M, et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19. N Engl J Med 383 (2020):120-128.
- Wang Y, Jin C, Wu CC, et al. Organizing pneumonia of COVID-19: Time-dependent evolution and outcome in CT findings. PLoS One 15 (2020): e0240347.
- Umbrello M, Formenti P, Nespoli S, et al. Effect of Different Corticosteroid Regimens on the Outcome of Severe COVID-19-Related Acute Respiratory Failure. A Retrospective Analysis. Journal of clinical medicine 10 (2021): 4847.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 75.63%
Acceptance Rate: 75.63%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
