Technical and Ethical Challenges in the Care of an Independent Nonagenarian with Critical Limb Ischemia
Article Information
Arash Fereydooni MS1, Neera Dahl MD, PhD2, Cassius Iyad Ochoa Chaar MD, MS3
1Yale University School of Medicine, New Haven, CT, USA
2Department of Internal Medicine, Division of Nephrology, Yale University School of Medicine, New Haven, CT, USA
3Section of Vascular Surgery, Department of Surgery, Yale University School of Medicine, New Haven, CT, USA
*Corresponding Author: Dr. Cassius Iyad Ochoa Chaar, Associate Professor of Surgery (Vascular), Yale School of Medicine, Yale New Haven Hospital, New Haven, CT, USA
Received: 02 January 2020; Accepted: 09 January 2020; Published: 31 January 2020
Citation: Arash Fereydooni, Neera Dahl, Cassius Iyad Ochoa Chaar. Technical and Ethical Challenges in the Care of an Independent Nonagenarian with Critical Limb Ischemia. Archives of Clinical and Medical Case Reports 4 (2020): 130-137.
View / Download Pdf Share at FacebookAbstract
Objective: Caring for elderly patients with peripheral artery disease is challenging given their complex anatomy and frail physiology. Despite advances in endovascular therapy, intervening on this patient population poses unique technical and ethical considerations. Present is a case that illustrates both the technical challenges and the ethical dilemma in the care of a 94-year old man with end stage renal disease treated for critical limb ischemia.
Methods: The medical record of patient was reviewed.
Results: Under local anesthesia and sedation, subintimal arterial flossing with antegrade-retrograde intervention was performed for recanalization of chronic total occlusion of superficial femoral artery. Patient healed his toe amputation wound at 5-week follow-up and was able to walk independently.
Conclusion: Advances in endovascular therapy provide effective treatment of very old patients with CLI. Discussing and setting realistic expectations with patients and their families is crucial to ensure the elderly are provided with better quality of life.
Keywords
Peripheral arterial disease; Functional Status; Retrograde access; Critical Limb Ischemia
Article Details
1. Introduction
The proportion of elderly patients in the United States keeps rising as the population over 85 years old is estimated to increase from 2.0% in 2017 to 4.5% in 2050 [1]. Challenges in delivering the optimal vascular care continue, particularly in this older population [2]. The advancement of endovascular intervention has provided less-invasive treatment options for high surgical risk patients. In fact, an endovascular-first approach has been advocated for revascularization in octogenarians as a better tolerated modality of treatment compared with open surgical bypass [3, 4]. Endovascular advances give patients the opportunity to live longer, but this might come at the cost of poor quality of life and significant emotional and financial burden to the patients and their support systems. Even though return to baseline is not always feasible, relieving symptoms and providing compassionate care is often possible. We present the case of a 94-year old independent patient with CLI.
2. Case Report
2.1 Presentation
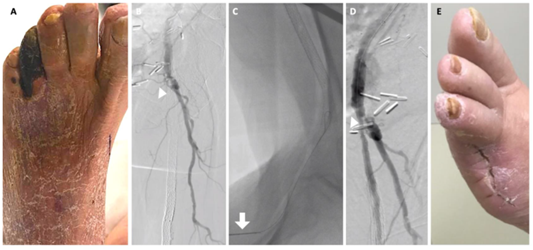
A 94-year-old man with end-stage renal disease on hemodialysis for the past 3 years, spinal stenosis, remote history of colon cancer requiring resection and prostate cancer requiring prostatectomy presented with 3-month-long worsening rest pain, non-healing left 4th toe gangrene and cellulitis of dorsum of left foot (Figure 1A). He had known peripheral artery disease and underwent left superficial femoral artery (SFA) stenting 15 years prior. His social history is significant for a prior smoking history of 135 pack-years. He was living independently in an assisted living facility and was functional until he developed the foot ulcer. He was treated conservatively with wound care, but his wounds progressed and he started complaining of rest pain.
On the left, there was progressive flattening of the pressure volume waves at the level of SFA and with no detectable signal thereafter. Computed tomography angiography showed complete occlusion of the left SFA stent extending from the SFA to the above-the-knee popliteal artery with distal reconstitution at the level of the popliteal artery.
The patient was seen by another specialist who recommended hospice or below knee amputation. After long discussions with him, his family and other providers involved in his care, several options were offered, including medical treatment alone, hospice care if his condition worsens, angiography with endovascular revascularization, open revascularization with a femoral-popliteal bypass or a below-the-knee amputation. The patient and his family opted in for endovascular revascularization.
2.2 Surgical techniques
Under local anesthesia and sedation, the right common femoral artery (CFA) was accessed and a pelvic angiogram showed patent iliac arteries. Selective angiogram of the left lower extremity showed patent CFA and profunda femoris artery and a totally occluded SFA with a stent (Figure 1B). There was reconstitution of the popliteal artery right above the knee and a single-vessel peroneal runoff that reconstituted the dorsalis pedis (DP) artery.
Under roadmap guidance, a NaviCross (Terumo Interventional Systems, Somerset, NJ) and a 0.035 Glidewire Advantage (Terumo Interventional Systems, Somerset, NJ) were used to engage the origin of the SFA stump. The wire and catheter were advanced subintimally around the old stents to the area of the popliteal artery where the artery reconstituted. However, reentry was not possible. The subintimal plane was very difficult to develop because of the prior stent; therefore, we decided not to use a reentry device.
The anterograde strategy was abandoned and instead a retrograde approach was attempted. The below-the knee popliteal artery was accessed under ultrasound guidance. An 0.018 wire (V18 wire, Boston Scientific, Marlborough, MA) was advanced into the occluded stents and a 0.018 Quick Cross (Spectranetics, Colorado Springs, CO) was advanced retrograde over the wire (Figure 1C). Selective angiography was performed confirming intraluminal placement of the wire. Using the Quick Cross and the 0.018 wire, we advanced through the occluded stent and passed the heavily calcified lesion at the proximal cap and enter into the true lumen of CFA. Next the wire was snared from the contralateral side. While flossing the wire, it exteriorized from both sides and the Quick Cross was exchanged for a 4 mm Sterling balloon (Boston Scientific, Marlborough, MA), and angioplasty of the stents and the above-knee popliteal artery was performed. Next, two Viabahn 6 mm × 250 mm stent grafts (Gore, Flagstaff, AZ) were deployed from the origin of the superficial femoral artery the popliteal artery at the level of the knee. The completion angiogram showed excellent flow through the SFA stent with no evidence of dissection, perforation, or residual stenosis (Figure 1D). The peroneal artery filled briskly all the way to the foot. Hemostasis was achieved by holding pressure on the popliteal artery for 30 minutes and deploying a 6-French Angio-Seal (Terumo Interventional Systems, Somerset, NJ) in the right groin.
Post-operatively, the patient recovered without complications. He had a palpable left DP pulse, and a strongly biphasic left PT pulse. Three weeks post-intervention, he underwent amputation of left 4th and 5th toes and was discharged to short-term rehabilitation.
2.3 Follow-up
On 5-week follow-up, the amputation site was healed (Figure 1E), the stents were patent with no residual stenosis on ultrasound and he was able to walk independently. After 6 weeks of rehabilitation, the patient went back to independent living. Nine months post-intervention, as patient’s functional status started declining, he decided to discontinue further hemodialysis. One week later, he passed away in his sleep after celebrating his 95th birthday with his family. Informed consent has been obtained from the patient’s family for publication of the case report and accompanying images.
Figure 1: Patient presented with (A) non-healing left 4th toe gangrene, cellulitis of dorsum of left foot. (B) Angiography showed patent left CFA and profunda femoris artery and a totally occluded SFA with a stent. Arrowhead denotes the origin of SFA. (C) In a retrograde approach, an 0.018 wire was advanced from below-the-knee popliteal artery into the occluded stents. Arrow denotes the needle at the below-the-knee popliteal artery access site. (D) The completion angiogram showed excellent flow through the SFA stent with no evidence of dissection, perforation, or residual stenosis. (E) The amputation site was healed at follow-up.
3. Discussion
This case represents a technical and ethical dilemma that vascular surgeons will increasingly face while caring for the growing population of very old patients. With more treatment options available, ethical consideration in revascularization treatment of the elderly patients has become an important issue. Elderly patients may need palliative care or customized management based on their functional and cognitive assessment, and age alone cannot determine therapy choices [5]. Functional status is an important predictor of mortality after open and endovascular lower extremity revascularization with infrainguinal bypass surgery [6-9]. In a recent study of elderly with CLI undergoing endovascular revascularization, functional status was found to be more significant predictor of morbidity and mortality than age [9]. A recent study on functional outcomes after lower extremity revascularization in nursing home residents showed little gain of function and a high mortality one year after surgery [10]. Nevertheless, ambulatory function, is usually not the primary goal of treatment as patients who undergo revascularization will mainly benefit from pain relief, wound healing, and prevention of major amputation.
Decisions about whether or not to treat advanced CLI in elderly patients with revascularization may pose an ethical dilemma. Communication with patients may be particularly challenging as palliative treatment rather than curative treatment becomes the main focus. Minimizing the impact of worsening quality of life by performing the least invasive procedure possible also requires that patient, family members, and treating physicians all agree on an assessment of the patient’s current functional status. It is therefore crucial to have open dialogue with the patient and the family involved in decision-making and set realistic goals of care. Often, the most feared outcome is prolongation of suffering and not death. Surgeons who want to offer information about quality of life and benefit of intervention are even more challenged by the paucity of data comparing survival beyond 30 days, quality of life, and function [11]. Measures of functional status, disability-free survival, days spent at home, or freedom from pain after surgery may provide information on outcomes that are clinically meaningful. Endovascular therapy is particularly attractive in this age group, as it is associated with relatively rapid recovery, short hospital-stay if needed, minimal pain and is less likely to impact baseline quality of life compared to open bypass or major amputation. As an alternative, palliative care is an option that is underutilized and understudied in surgical patients but preferred in patients who have a poor quality of life at baseline [11]. Endovascular innovation makes it possible to push the boundaries of care for the aging population and vascular surgeons will be inevitably crossing the blurred borderlines between clinically appropriate and ethically acceptable care. Surgeons should then be trained to discuss options such as no treatment and palliative care in addition to minimally invasive procedures. In our case, the patient was able to return to independent living. He deliberately withdrew from dialysis because he did not want to live beyond his 95th birthday.
Despite the significant improvements in endovascular technology, complex arterial lesions pose significant technical challenges in the endovascular treatment of advanced arterial occlusive disease in the elderly. Recanalization of a chronic total occlusion (CTO) of the SFA may fail in up to 25% of attempts [12]. The common reasons for failure are flush SFA occlusion, occluded stents, wire perforation, and re-entry failure [13, 14]. By using a retrograde popliteal artery approach, the guide wire can pass more easily through the softer distal end of CTO. Other benefits include enhanced maneuvering because of the proximity of target lesion and access site, better safety profile in those with inguinal scars or obese patients [15], and reduced costs compared with the use of re-entry devices.
Several publications have demonstrated a high success rate and safety of retrograde transpopliteal technique, with reported 1-year primary patency rate of 65.8-89.5% [16-19]. This approach requires the patient to be repositioned to a prone position during the procedure, which is challenging and inconvenient for both patient and surgeon. An alternative method of performing the transpopliteal approach with the patient supine is to access the popliteal artery with the knee flexed and rotated externally [20-22]. Retrograde puncture of the distal SFA, through anteromedial access route into the distal thigh without knee flexion is another alternative with 96% technical success rate [23]. However, the utility of this technique is limited to SFA lesions not extending beyond the adductor canal. As demonstrated in our case, a dual femoral–popliteal approach in the supine position is also another option [24]. Recently, an anterolateral popliteal puncture technique to treat femoropopliteal CTO extending distally to the P3 segment of popliteal artery with 100% technical success rate of 100% has been reported [25, 26]. In this approach, the patient remains in supine position, with no requirements for rotation or flexion of the limb, and a 21-G, 9-cm angiographic needle (Cook Medical Inc, Bloomington, Indiana) is used to establish retrograde access to either the tibioperoneal trunk or the P3 segment of the popliteal artery. Reported complications due to the transpopliteal approach range from 2.5 to 5.2% [27] and most commonly are puncture site hematoma, pseudoaneurysm, and arteriovenous fistula [27, 28].
4. Conclusion
Advances in endovascular therapy provide effective treatment of very old patients with CLI. Discussing and setting realistic expectations with patients and their families is crucial. With the rapid growth of the aging population, further research and studies are needed to personalize vascular care and ensure it is providing the elderly with better quality of life.
Acknowledgments
None
Conflicts of Interest
Authors have no conflicts of interest to disclose.
Funding
There was no research funding for this work.
Data Availability Statement
All data generated or analyzed during this study in this article (and its Supplementary Material file) are openly available from the corresponding author on reasonable request.
References
- Bureau USC. Population Estimates and 2017 National Projections (2017).
- Veith FJ. The society for vascular surgery: A look at the future. Journal of Vascular Surgery 24 (1996): 144-147.
- Brosi P, Dick F, Do DD, et al. Revascularization for chronic critical lower limb ischemia in octogenarians is worthwhile. Journal of Vascular Surgery 46 (2007): 1198-1207.
- Dosluoglu HH, Lall P, Cherr GS, et al. Superior limb salvage with endovascular therapy in octogenarians with critical limb ischemia. Journal of Vascular Surgery 50 (2009): 305-316.e2.
- Shah P, Aung TH, Ferguson R, et al. Ethical Consideration in Wound Treatment of the Elderly Patient. The journal of the American College of Clinical Wound Specialists 6 (2016): 46-52.
- Crawford RS, Cambria RP, Abularrage CJ, et al. Preoperative functional status predicts perioperative outcomes after infrainguinal bypass surgery. Journal of Vascular Surgery 51 (2010): 351-359.
- Arvela E, Venermo M, Söderström M, et al. Infrainguinal percutaneous transluminal angioplasty or bypass surgery in patients aged 80 years and older with critical leg ischaemia. BJS 98 (2011): 518-526.
- Saarinen E, Vuorisalo S, Kauhanen P, et al. The Benefit of Revascularization in Nonagenarians with Lower Limb Ischemia is Limited by High Mortality. European Journal of Vascular and Endovascular Surgery 49 (2015): 420-425.
- Dinga Madou I, Slade MD, Orion KC, et al. The Impact of Functional Status on the Outcomes of Endovascular Lower Extremity Revascularization for Critical Limb Ischemia in the Elderly. Ann Vasc Surg 45 (2017): 42-48.
- Oresanya L, Zhao S, Gan S, et al. Functional outcomes after lower extremity revascularization in nursing home residents: a national cohort study. JAMA internal medicine 175 (2015): 951-957.
- Lilley EJ, Cooper Z, Schwarze ML, et al. Palliative Care in Surgery: Defining the Research Priorities. Annals of Surgery 267 (2018): 66-72.
- Bausback Y, Botsios S, Flux J, et al. Outback catheter for femoropopliteal occlusions: immediate and long-term results. Journal of endovascular therapy: an official journal of the International Society of Endovascular Specialists 18 (2011): 13-21.
- Met R, Van Lienden KP, Koelemay MJW, et al. Subintimal Angioplasty for Peripheral Arterial Occlusive Disease: A Systematic Review. CardioVascular and Interventional Radiology 31 (2008): 687-697.
- Montero-Baker M, Schmidt A, Bräunlich S, et al. Retrograde Approach for Complex Popliteal and Tibioperoneal Occlusions. Journal of Endovascular Therapy 15 (2008): 594-604.
- Evans C, Peter N, Gibson M, et al. Five-year retrograde transpopliteal angioplasty results compared with antegrade angioplasty. Annals of the Royal College of Surgeons of England 92 (2010): 347-352.
- Matsumi J, Takada T, Moriyama N, et al. Initial and Long-Term Results of a Microcatheter-Based Retrograde Approach for the Endovascular Treatment of Chronic Total Occlusion in Iliac or Femoropopliteal Arteries. Annals of Vascular Surgery 41 (2017): 176-185.
- Dumantepe M. Retrograde Popliteal Access to Percutaneous Peripheral Intervention for Chronic Total Occlusion of Superficial Femoral Arteries. Vascular and Endovascular Surgery 51 (2017): 240-246.
- Brountzos EN, Moulakakis KG, Avgerinos E, et al. Retrograde Transpopliteal Approach of Iliofemoral Lesions. Vascular and Endovascular Surgery 45 (2011): 646-650.
- Ye M, Zhang H, Huang X, et al. Retrograde popliteal approach for challenging occlusions of the femoral-popliteal arteries. Journal of Vascular Surgery 58 (2013): 84-89.
- Kawarada O. Miniaturized Retrograde Popliteal Approach in a Supine Patient. Journal of Endovascular Therapy 18 (2011): 510-512.
- Kawarada O, Yokoi Y. Retrograde 3-French Popliteal Approach in the Supine Position after Failed Antegrade Angioplasty for Chronic Superficial Femoral Artery Occlusion. Journal of Endovascular Therapy 17 (2010): 255-258.
- Fanelli F, Lucatelli P, Allegritti M, et al. Retrograde Popliteal Access in the Supine Patient for Recanalization of the Superficial Femoral Artery: Initial Results. Journal of Endovascular Therapy 18 (2011): 503-509.
- Schmidt A, Bausback Y, Piorkowski M, et al. Retrograde recanalization technique for use after failed antegrade angioplasty in chronic femoral artery occlusions. Journal of endovascular therapy: an official journal of the International Society of Endovascular Specialists 19 (2012): 23-29.
- Shi W, Yao Y, Wang W, et al. Combined Antegrade Femoral Artery and Retrograde Popliteal Artery Recanalization for Chronic Occlusions of the Superficial Femoral Artery. Journal of Vascular and Interventional Radiology 25 (2014): 1363-1368.
- Silvestro M, Palena LM, Manzi M, et al. Anterolateral retrograde access to the distal popliteal artery and to the tibioperoneal trunk for recanalization of femoropopliteal chronic total occlusions. Journal of Vascular Surgery 68 (2018): 1824-1832.
- Tan M, Urasawa K, Koshida R, et al. Anterolateral Popliteal Puncture Technique: A Novel Retrograde Approach for Chronic Femoropopliteal Occlusions. Journal of Endovascular Therapy 24 (2017): 525-530.
- Noory E, Rastan A, Sixt S, et al. Arterial Puncture Closure Using a Clip Device after Transpopliteal Retrograde Approach for Recanalization of the Superficial Femoral Artery. Journal of Endovascular Therapy 15 (2008): 310-314.
- Yanagita Y, Noda K. Incidence and risk factors of vascular complications following endovascular treatment of peripheral arterial disease via the popliteal artery. Cardiovascular Intervention and Therapeutics 26 (2011): 209-214.


 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
