A Preventable Maternal Death Case Report in Haho Health District, Togo, 2018
Tchalla A. Agballa ME1*, Akara EM1, Tchandana Makilioube2, Bakonde HE3, Bate Lare Palemague4, Yao Kassankogno4
1Direction Préfectorale de la Santé de Haho, Centre Hospitalier Préfectoral de Notsè, Togo
2Division de la Santé Maternelle, Infantile et de la Planification Familiale, Ministère de la santé et de l’hygiène publique, Togo
3Université Cheik Anta Diop Dakar, Sénégal
4Université de Lomé, Togo
*Corresponding Author: Dr. Tchalla Abalo Agballa Mébiny-Essoh, Direction Préfectorale de la Santé de Haho, Centre Hospitalier Préfectoral de Notsè, Togo
Received: 24 Sep 2019; Accepted: 14 October 2019; Published: 03 December 2019
Article Information
Citation: Tchalla A. Agballa ME, Akara EM, Tchandana Makilioube, Bakonde HE, Bate Lare Palemague, Yao Kassankogno. A Preventable Maternal Death Case Report in Haho Health District, Togo, 2018. Archives of Clinical and Medical Case Reports 3 (2019): 712-717.
View / Download Pdf Share at FacebookAbstract
From 1990 to 2015, maternal mortality has decline by 43.9 per cent worldwide. In sub-Saharan Africa countries including Togo, it’s still a great concern. Sustainable Development Goals recommend to achieve a maternal mortality ratio of less than 70 maternal deaths per 100,000 live births by 2030. We report a case of maternal death of a Christian pregnant woman that occurred in Haho health district in 2018. Data were collected through a review of registers, medical and antenatal records and verbal autopsy. The deceased suffered of severe pre-eclampsia like during her two previous pregnancies that ended with two stillbirths, but this time around she could not survive it despite the six antenatal visits with a gynaeco-obstetrician. Actually, she had the strong believe that the two stillbirths was uncommon and a result of a spell cast on her, and that only her faith through prayers could deliver her. Therefore, she did not comply with her reference to a hospital with a surgical service for a cesarean delivery. Her death was preventable. There is a need to strengthen patients’ therapeutic education and communication around diseases especially during pregnancies in order to help them know what faith cannot help achieve.
Keywords
<p>Maternal death; Severe pre-eclampsia; Faith, Haho; Togo</p>
Article Details
1. Introduction
Since the beginning of the 21st century, world leaders have committed that no woman should not die while trying to give birth [1]. Therefore, founds have been made available to support any action that would help achieve this sustainable development goal. Many progresses have been made and the incidence of maternal deaths have declined from 987 per 100,000 live births in 1990 to 546 per 100,000 live births in 2015 in sub-Saharan Africa [1, 2]. Despite this commitment, there is still some cases of maternal deaths that usually call for many interrogations. A part from the common and principal causes of maternal deaths known, there are some multifactorial reported maternal deaths that could be prevented [3]. One of them in the evolving context of social disparities in low- and middle-income countries, is the fact that people have more and more to rely on their faith to get heal from their diseases. On the process, out of their strong believe on their faith, some people use to die while it was possible to save them by implementing known therapeutic protocols that were proven to work on others. One of the diseases in pregnant women that has a protocol of treatment is the pre-eclampsia [4]. More and more pregnant women survive it if there is not any other specific comorbidity add to it. But unfortunately, the present case we are reporting, though she has no comorbidity associated to her pre-eclampsia did not survive it.
2. Case Presentation
The deceased, Miss D.A. was third time gravid with an history of two stillbirths during her last two pregnancies. She was a fatherless of 25-year-old, of primary school educational level, seamstress of christian religion, living in couple for three years at Adakpamé in Health District No. 2 (HD-II) in Lomé. The present pregnancy was of 37 weeks + 3 days according to the date of her last menstrual period at the date of her death. She first attended Adakpame’s hospital for antenatal consultation on March 15, 2018 when the pregnancy was 12 weeks. She later on attended six-time antenatal consultation (Table 1). After the first antenatal consultation the deceased was transferred from the midwife's consultation to that of the gynaeco-obstetrician for poor obstetrical history and short inter-reproductive interval. During her follow-up, the blood pressure (BP) started rising (130/80 mmHg) without detectable albuminuria at 30 weeks term and she was prescribed medical rest and etifoxine hydrochloride twice daily. At her last attendant on September 5, 2018, her BP was 150/90 mmHg with an albuminuria above 10 grams per liter, important lower limbs edema, weakness and breathlessness. A diagnosis of severe pre-eclampsia was established on that base and Miss D.A. was directed to Bè hospital in Health District No. 3 (HD-III) that have surgical facilities for urgent care and caesarean section (Figure 1).
|
Dates of antenatal |
Blood Pressure (mmHg) |
Weight (kg) |
Uterine height (cm) |
Albuminuria |
|
|
Systolic |
Diastolic |
||||
|
March 15, 2018 |
110 |
70 |
65 |
- |
undetectable |
|
April 18, 2018 |
110 |
70 |
68 |
- |
undetectable |
|
May 18, 2018 |
100 |
60 |
68 |
18 |
undetectable |
|
June 20, 2018 |
110 |
60 |
69 |
24 |
undetectable |
|
July 18, 2018 |
130 |
80 |
73 |
29 |
undetectable |
|
August 17, 2018 |
140 |
90 |
77 |
30 |
undetectable |
|
September 5, 2018 |
150 |
90 |
78 |
30 |
>10g/l |
Table 1: Records of parameters during antenatal consultation of Miss D.A.
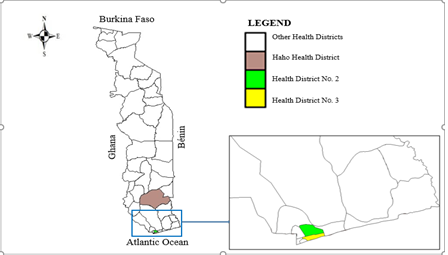
Figure 1: Case study area and pathway.
She was prescribed before being transferred, methyldopa three time daily and magnesium twice daily in addition of all the systematic supplementations during a pregnancy that she has been taking since the beginning of this pregnancy (Iron daily, and Sulfadoxine-pyrimethamine monthly to prevent malaria). Instead of going to Bè’s hospital, in the evening of the same day and out of the knowing of her husband, the deceased went to a prayer camp named “Jesus is the solution” located at Kpové in Haho health district, about 75 miles far away from Lomé, her usual residence. It was in that camp and during the night prayers, that she had generalized tonic and clonic seizures around 5am on September 06, 2018. She was carried to Haho’s district hospital where she was admitted at 9:25 am. The initial checking on her by maternity team at Haho’s district hospital has revealed a BP at 150/10 mmHg, albuminuria above 10 grams per liter and an unquoted state of coma with restlessness. A diagnosis of an eclamptic coma was establish and a treatment made of magnesium sulfate (4 grams intravenous + 10 grams intramuscular) and nicardipine (20 milligrams through slow perfusion) according to the national protocol of management of eclampsia, was immediately initiated and it is while she was undergoing resuscitation measures before being admitted in the operating room for caesarean section that she died at 9:46 am.
When questioned, the goodwill who carried the deceased from the prayer camp to the hospital said: “this lady, I don’t know her, I noticed her yesterday during the prayers as she was pregnant; we were still praying when she felt down and we prayed harder until she calmed down. But as she was pregnant and I saw her still on the ground and nobody cared about it, I just decided to take her to a hospital; I was just trying to help”.
After investigation, maternity staff of Haho’s district hospital found out that the methyldopa and magnesium prescribed at Bè hospital were bought but still untouched in their packaging. The family of Miss D.A. was met on August 02, 2019 for further details. They reported that the deceased was strongly convinced that the two stillbirth she had in the past were linked to a spell cast on her and that only prayers can save her during this new pregnancy so that she will be able to give birth. She tried several times to go to the prayer camp “Jesus is the solution” because she overheard that all problems even her own can be solve there, but her husband never allow her. The husband even states: “My wife was very attached to the idea of ??a spell cast on her responsible of her repeated stillbirths, and I do not know why despite I forbid her going to this prayer camp, and I even bought the medication prescribed at Adakpame’s hospital and give her money to attend the referral center, she stubbornly went there, and I have to be called by people from Haho’s district hospital that my wife is dead, it hurts me but this is life”.
3. Discussion
The death of Miss D.A. could be prevented. Pre-eclampsia incidence in pregnancies is still increasing especially in women that have risk factors or predisposing factors [5] but the proportional morbidity imputable to pre-eclampsia is decreasing [6, 7]. This is because the treatment and management of pre-eclampsia has known a lot of progress and is more codified [4, 8]. There are many evidences that shows that the protocols to treat pre-eclampsia, if initiated on time, helps prevent unfavorable outcomes like eclampsia and more, maternal deaths [4]. In this case the patient died because she did not attend the referral hospital on time and she did not take the pretransfer medication. When analyzed carefully, all this has happened because in the first place, the deceased has the strong belief that her case was not a treatable one and that only prayers to her lord could help her deliver safely this time around as she has been in the same clinical presentation during her last pregnancies which ended with two stillbirth. Secondly, in the prayer camp, when the deceased starts seizing, people around her should have taken her quickly to the hospital that she may have survive; instead, they were still praying assuming this seizures were the result of their prayers and that the devilish in her responsible of her condition during pregnancies, was being thrown out of her, and this, till she stops seizing as reported by the goodwill. These seizures that appeared are a common complication of unmanaged severe pre-eclampsia which has an established protocol of treatment in accredited hospitals in the country; and many patients in that situation have survive it [9]. From 5am she starts seizing to 9:25am the case could not reach Haho’s district hospital which is normally reachable in 30 minutes time maximum from the prayer camp; the deceased could have been brought to the hospital in 30 minutes time since 5am she started seizing. This point out two situations that may have resulted in the unfavorable outcome: the late request for medical services or facilities by patients in our conditions of low- and middle-income countries [10, 11] even if they do not exist or they exist and also the lack of information and knowledge concerning what should be considered as an emergency or not [2]. The phenomenon of new churches in sub-Saharan countries, created anyhow without control and regulations, pretending that they have the solution to all the problems [12], even clinical known diseases with establish treatment is an important issue in this case presentation. The importance of spirituality or faith in a patient psychological stability, essential for his organic illness recovery have been demonstrated [13, 14]; apart from that evidence, patients have to know when to overcome their faith and refer to medical treatment of their clinical conditions. Besides, scientific reasoning and religious reasoning called faith, complement one another in one individual [15, 16].
4. Conclusion
The case reported here has shown the limit that faith should not cross in order not to be detrimental for the patient, for, there are evidences of what faith and spirituality can help stabilize in one patient and what they cannot help for. It has also point out some organizational lacks in healthcare systems of low- and middle-income countries like Togo that happened to have caused this maternal death in a condition of severe pre-eclampsia. Therefore, it is important for healthcare authorities and healthcare practitioners to emphasize on therapeutic education and more explanation to patients about their conditions each time it is right, on a multidisciplinary basis. It is also important that spiritual leaders should consider trying to collaborate more with healthcare practitioners to save lives on a holistic treatment approach of any person they get in contact with.
Competing Interests
The authors declare that they have no competing interests.
Ethical Consideration
This study has the approval of Haho health district coordination. The deceased family members encountered during the investigation have given informed consent for this case report.
References
- Alkema L, Chou D, Hogan D, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet 387 (2016): 462-474.
- World Health Organization. Maternal Mortality. http://www.who.int/mediacentre/factsheets/fs348/en/ (2016).
- Say L, Chou D, Gemmill A, et al. Global Causes of Maternal Death: A WHO Systematic Analysis. Lancet Global Health 2 (2014): e323-e333.
- Duhig K, Vandermolen B, Shennan A. Recent advances in the diagnosis and management of pre-eclampsia. (doi: 10.12688/f1000research.12249.1) (2018): 242.
- Fauvel JP. Hypertensions et grossesse : aspects épidémiologiques, définition. La Presse Médicale 45 (2016): 618-621.
- Thornton C, Dahlen H, Korda A, et al. The Incidence of Preeclampsia and Eclampsia and Associated Maternal Mortality in Australia From Population-linked Data Sets. American journal of obstetrics and gynecology (2013): 35.
- Auger N, Luo ZC, Nuyt AM, et al. Secular Trends in Preeclampsia Incidence and Outcomes in a Large Canada Database: A Longitudinal Study Over 24 Years. Canadian Journal of Cardiology 32 (2016): 987e15-987.e23.
- Turner JA. Diagnosis and management of pre-eclampsia: an update. International Journal of Women’s Health 2 (2010): 327-337.
- Fontenot MT, Lewis DF, Frederick BJ, et al. A prospective randomized trial of magnesium sulfate in severe preeclampsia: use of diuresis as a clinical parameter to determine the duration of postpartum therapy. American Journal of Obstetrics and Gynecology 192 (2005): 1788-1793.
- Twum-Danso NA, Akanlu GB, Osafo E, et al. A nationwide quality improvement project to accelerate Ghana’s progress toward Millennium Development Goal Four: design and implementation progress. Int J Qual Health Care 24 (2012): 601-611.
- Ngabo F, Nguimfack J, Nwaigwe F, et al. Designing and implementing an innovative SMS-based alert system (RapidSMS-MCH) to monitor pregnancy and reduce maternal and child deaths in Rwanda. Pan Afr Med J 13 (2012): 31.
- Adedibu BA. The changing faces of African Independent Churches as development actors across borders. HTS Teologiese Studies/Theological Studies 74 (2018): 4740
- Hosseini M, Davidson PM, Khoshknab MF, et al. Spiritual and religious interventions in healthcare: An integrative review. Iranian Rehabilitation Journal 11 (2013).
- Ntantana A, Matamis D, Savvidou S, et al. The impact of healthcare professionals’ personality and religious beliefs on the decisions to forego life sustaining treatments: an observational, multicentre, cross-sectional study in Greek intensive care units. BMJ Open 7 (2017): e013916.
- Gingras Y. L’Impossible dialogue. Sciences et religions?. Paris, Presses universitaires de France 422 (2016).
- Galadari A. Science vs. Religion: The Debate Ends. The International Journal of Science in Society 2 (2011).


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 75.63%
Acceptance Rate: 75.63%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
