A Strange Case of Recurrent Pain and Swelling in the Upper Limbs
Roberta Barolo, MD*, Giulia Pruccoli, MD, Carlotta Covizzi, MD, Nathalie Bini, MD, Federica Mignone, MD, Francesco Licciardi, MD, Erika Silvestro, MD, Silvia Garazzino, MD
Regina Margherita Children’s Hospital, Turin, Italy
*Corresponding Author: Roberta Barolo, MD, Regina Margherita Children’s Hospital, Turin, Italy.
Received: 25 October 2023; Accepted: 29 November 2023; Published: 22 December 2023
Article Information
Citation: Roberta Barolo, Giulia Pruccoli, Carlotta Covizzi, Nathalie Bini, Federica Mignone, Francesco Licciardi, Erika Silvestro, Silvia Garazzino. A Strange Case of Recurrent Pain and Swelling in the Upper Limbs. Archives of Clinical and Medical Case Reports. 7 (2023): 424-427.
View / Download Pdf Share at FacebookAbstract
Myositis ossificans (MO) is a benign and rare condition characterized by the heterotopic non-neoplastic bone formation within skeletal muscle and/ or soft tissues. There are 3 forms of MO of which the traumatic is the most frequent, while non-traumatic MO is exceptionally rare especially in pediatric age, as evidenced by the few studies published in the literature. MO mainly affects adolescents and young adults; lesions are usually found in muscles of the lower and upper limbs. Major injury and minor repeated trauma are considered the most common etiological hypotheses. The presenting symptoms are usually pain, the presence of a soft tissue mass with tenderness over the swelling, overlying hot and erythematous skin. MO should be differentially diagnosed with other benign lesions, with malignant lesions and infections. Given the rarity of this condition, early diagnosis can be difficult to achieve but is fundamental to avoid unnecessary investigations and treatments and to reach a successful outcome. Ultrasonography, X-ray and MRI can show the characteristic pattern of calcification of MO; biopsy is not necessary if radiographic investigations allow definitive diagnosis. Therapies for MO include conservative treatment and surgical excision, the latter indicated in cases of neurovascular impairment, functional limitations, major aesthetic alteration.
We present the case of a 14-year-old girl with non-traumatic MO in the forearm presenting with long lasting pain and swelling; the clinical presentation, diagnostic process, radiological findings and management of this unique case are discussed.
Keywords
<p>Myositis ossificans; Non-traumatic; Forearm; Pediatric</p>
Article Details
1. Introduction
Myositis ossificans (MO) consists in a process of heterotopic non-neoplastic bone formation in skeletal muscle and/or soft tissues. It’s considered a benign and rare lesion and it’s classified in three different forms: progressive MO, a genetic severe and generalized form; a non-traumatic or pseudomalignant MO, which occurs in the absence of any trauma and may follow burns or show up in patient with haemophilia; circumscripta or traumatic MO, which is the most frequent form and related to a direct trauma [1]. It can be observed at any age but it mainly affects adolescents and young adults [2]. Lesions are more frequently found in muscles of the lower and upper limbs, but can occasionally involve other sites (abdominal muscles, paravertebral muscles, etc) [3].
Initial clinical presentation is generally characterized by a painful soft tissue mass with tenderness over the swelling, overlying hot and erythematous skin; whether it affects a joint, joint pain and increased joint stiffness can be observed [4]. As a result of bone tissue formation in a heterotopic site, a palpable osseous mass can be appreciated and should be differentially diagnosed with malignant lesions. Given the rarity of this condition, early diagnosis can be difficult to achieve but is fundamental to avoid unnecessary investigations and treatments and to reach a successful outcome.
This report describes a case of non-traumatic MO in a 14-years-old girl presenting with long lasting pain and swelling at the right forearm.
2. Case Presentation
A 14 years-old girl presented several times to the emergency department complaining about right forearm swelling and pain. The patient came from Mali and has been living in Italy for 4 years; she didn’t report recent trips abroad. There was no relevant family or personal history. Two and a half years earlier the girl had experienced pain and swelling of the left forearm, that lasted for about 6 months.
At clinical examination an indurated swelling lesion intensely painful on palpation localized on the left forearm was recorded; overlying skin was normothermic and non-erythematous. Swelling and pain at left elbow with warm overlying skin and associated functional impotence was also recorded. The girl did not recon a precipitating event or an even minimal trauma to the left forearm. To better understand the nature of left forearm lesion the following investigations were performed:
- blood test: a minimum increase of creatine phosphokinase (CPK) was found, negative indices of inflammation (C-reactive protein - CRP - and erythrocyte sedimentation rate - ESR);
- smear of peripheral blood: negative for blasts; negative bone marrow immunocytofluorimetry and myeloculture;
- left forearm X-ray: negative for bone lesions;
- doppler ultrasound of left forearm: no signs of deep venous thrombosis;
- soft tissue ultrasound: in corrispondence with the lesions at the left forearm presence of thickening of the subcutaneous tissue, the largest approximately 23 x 4 mm, characterized by finely inhomogeneous hyperechogenic ecostructure and blurred margins. This finding was referable to an inflammatory lesion (fasciitis or miositis);
- MRI of left forearm: hyperintensity in the T2-weighted sequence, to which corresponds discrete enhancement after contrast agent administration, at the level of the proximal tract of the deep finger flexor muscle and adjacent subcutaneous adipose tissue. This finding could be referable to a sign of inflammation.
In the diagnostic hypothesis of an infectious lesion an antibiotic therapy (amoxicillin- clavulanate acid and clarithromycin), nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids were administered, but without benefit. Approximately 6 months after the onset of left forearm symptoms the patient reported their complete spontaneous resolution with appearance of similar symptomatology in the right forearm, where she experienced for 2 years alternating periods of swelling and pain worsening with periods of improvement without complete disappearance.
In June 2023 she came to the emergency department for worsening pain and swelling at the right forearm (Figure 1A). The following investigations were performed: doppler ultrasound and X-ray of right forearm resulted negative; soft tissue ultrasound with the finding of an extensive inhomogeneously echogenic area in the subfascial site on the ulnar side of right forearm approximately 10 cm in size, probable referred to a fluid collection with imbibition of neighboring muscles. In the suspicion of infectious pathology an endovenous antibiotic therapy with teicoplanin and amoxicillin-clavulanate acid was administered with little benefit and a rehabilitation project was set up, with partial benefit on pain and swelling. The patient was then discharged; at home swelling and pain improved for one month, but then increased again without a known trauma. She was therefore referred again to the emergency department where an ultrasound of the forearm was repeated and showed an image referable to fascitis or blood collection in the pronator and flexo radialis muscle of the right forearm. At blood tests complete blood count, indices of inflammation and coagulation tests were within the normal range. An intravenous therapy with cefotaxime + clindamycin and steroid therapy with betamethasone was administered and a right forearm MRI was performed (Figure 1B). An orthopedic evaluation was then requested and a plaster shower was placed; the girl was then discharged home with indication to keep the limb in unloading and to take NSAIDs oral therapy.
After two days the patient reported worsening pain in the right forearm and she went again to the emergency room where the plaster shower was removed. At physical examination of right forearm, on the medial surface, a painful swelling with warm overlying skin and without skin lesions was recorded; an ultrasound was made with the finding of images of dystrophic calcifications in the adductor muscle and persistence of hypercogenicity of muscle structures. An X-ray confirmed gross calcification images (Figure 1C). In light of the clinical course and the findings at instrumental examinations, the diagnostic suspicion of myositis ossificans was raised. After collegial discussion including orthopedic, radiology, rheumatology, and oncology specialists, it was decided that the patient should continue NSAIDs therapy at home.
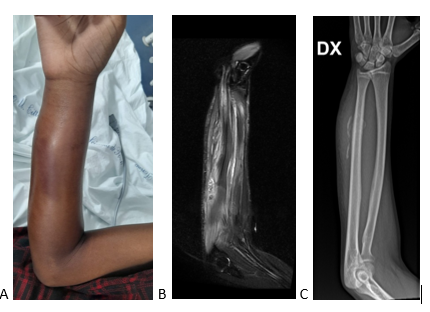
Figure 1: (A) Painful swelling at right forearm, with warm overlying skin and without skin lesions. (B) Right forearm MRI showing an area of inhomogeneous and predominantly fluid appearance (approximately 81 X 20 mm) with hyperintense cercine after administration of contrast agent and associated superficial tissue edema, in correspondence to the muscles of the anterior compartment of the right forearm (mainly the flexors and round pronator): this finding was consistent either with bleeding or a flogistic area. (C) Right forearm X-ray showing gross calcification images in the muscular framework of the right forearm associated with modest periosteal reaction in the mid-diaphyseal ulnar site.
During the various hospitalizations the following investigations were performed to rule out possible differential diagnoses and resulted all negative:
- infectious investigations: serology for Bartonella, blood cultures, blood parasites research (including heartworm), Quantiferon-TB test;
- coagulation investigations: comprehensive thrombophilic screening, coagulation factors dosage, prothrombin time, fibrinogen dosage, platelet aggregation test, Von Willebrand Factor dosage and activity;
- calcium-phosphorus metabolism;
- rheumatologic/autoimmune investigations: search for anti-nuclear antibody, extractable nuclear antigens, anti-neutrophil cytoplasmic antibodies, anti-myositis antibodies, anti-hydroxy antibodies methyl glutaryl coenzyme A, C3 and C4 dosage;
- hemoglobin balance: presence of band in heterozygosity referable to HbS (healthy HbS carrier).
After the start of anti-inflammatory therapy the painful symptoms have gradually improved until complete resolution with a concomitant reduction of edema in the rest of the forearm and reduction. On clinical and instrumental follow-up one month later ultrasound and X-ray showed stable calcification images while at physical examination the hard tumefaction was not increased in size, it wasn’t painful, overlying skin was non tender and non erythematous and swelling was not present. Less than a month after the last follow-up visit, however, the patient was again admitted to hospital for increased pain; on X-ray there was evidence of extension of the right forearm calcifications. Steroid therapy was then started, which is still ongoing.
3. Discussion
Non-traumatic MO is rare, especially in pediatric age, as evidenced by the few studies published in the literature. To our knowledge, only one clinical case has been published describing a non-traumatic MO in forearm in a pediatric patient who complained swelling and the presence of a lesion since 1 year [5]. However the case we described differs from the one already published for migrating and inconstant symptomatology over time and the late positivity of radiological investigations that made the diagnosis difficult.
MO is a process of heterotopic bone formation. Among all the proposed etiological hypotheses, major injury and minor repeated trauma are considered the most common; probably trauma is followed by inflammation that causes the release of periostal cells and growth factors into muscle or soft tissue [6, 7]. Patients can be asymptomatic; otherwise the presenting symptoms are pain, sensitive focal swelling and erythematous skin overlying the area affected by the ossification process [8]. Our patient presented with long lasting and recurrent episodes of pain and swelling in both the right and left forearm.
MO is a benign lesion that rarely grow after the initial diagnosis and can have a self-limited course going through spontaneous regression after several months [3]. Conditions that primarily should be considered in the differential diagnosis include progressive fibrodysplasia ossificans, sarcoma (osteosarcoma, synovial sarcoma, fibrosarcoma), osteochondroma, post-traumatic periostitis, ossified fibromixoid tumor and infections; when MO affects a joint it should be put in differential diagnosis with inflammatory arthritis [9]. Imaging techniques are important to rule out malignancies or infectious processes, but they are not always direct; MO goes through various maturation stages and in early stages there may be minimal or no calcifications on radiological investigations [3]. Nevertheless ultrasonography, conventional X-ray and MRI can show images that allow differentiating MO from a malignancy and are the best imaging for follow-up, too; in fact the pattern of calcification is usually different between MO and a malignant lesion: for example in MO the calcification start from the periphery and then develop to the center, while in osteosarcoma calcification will be from the center to the periphery [10,11]. In our case many investigations were performed with the aim of ruling out infectious etiologies, coagulation pathologies, immuno-rheumatological pathologies, haemoglobinopathies and all these investigations were necessary before arriving at a definitive diagnosis because radiological investigations were only diriment several months after the onset of symptomatology. Furthermore, multiple empirical antibiotic therapies have been administered in doubt of an infectious disease, without benefit on symptoms.
If radiographic investigations allow definitive diagnosis, biopsy has not to be performed; otherwise a biopsy is necessary. Histologic findings suggesting MO are degenerating muscle fibers, low cellularity, absence of nuclear atipia, benign proliferating fibroblasts, presence of immature and mature trabeculae, myxoid stroma with osteoid, ossification [12, 13]. In our case biopsy was not performed because the clinical development and radiological investigations were suggestive for MO and also because of the difficulty in performing a biopsy in such a deep anatomical site.
Therapies for MO include conservative treatment (such as rest, the application of cold packs, NSAIDs, physiotherapy) and surgical excision; the latter is usually indicated in cases of neurovascular impairment, functional limitations, major aesthetic alteration [6]. Our patient continued physiotherapy and was treated conservatively initially with NSAIDs and later with steroids, due to a new recurrence of pain and swelling.
4. Conclusions
MO is a benign process of non-neoplastic ossification in soft tissues and muscles and it is sometimes difficult to be distinguished from a malignant lesion. Non-traumatic MO is not very common but when a child presents with a painful soft-tissue swelling it has to be considered in the differential diagnosis together with malignant lesions and infections. A thorough medical history and physical examination, laboratory tests, and radiologic examinations are crucial for an appropriate differential diagnosis. However, if a definite diagnosis cannot be reached, a biopsy with histological analysis of the specimen should be performed. Therapy involves the use of conservative treatments or surgical excision in selected cases.
Declaration
The authors declare no conflicts of interest.
References
- Gindele A, Scwamborn D, Tsironis K, Benz-Bohm G. Myositis ossificanstraumatica in young children: report of three case and review of literature. PediatrRadiol 30 (2000): 451-459.
- Nishio J, Nabeshima K, Iwasaki H, Naito M. Non-traumatic myositis ossificans mimicking a malignant neoplasm in an 83-year-old woman: a case report. J Med Case Rep 4 (2010): 270.
- Lau J, Hartin CW, Ozgediz DE. Myositis ossificans requires multiple diagnostic modalities. J PediatrSurg 47 (2012): 1763-1766.
- Sferopoulos NK, Kotakidou R, Petropoulos AS. Myositis ossificans in children: a review. Eur J OrthopSurgTraumatol 27 (2017): 491-502.
- Say F, Coskun S, Bülbül M, Alici Ö. Myositis ossificans on the forearm in a 10-year-old girl. J PediatrOrthop B 24 (2015): 223-225.
- Micheli A, Trapani S, Brizzi I, et al. Myositis ossificanscircumscripta: a paediatric case and review of the literature. Eur J Pediatr 168 (2009): 523-529.
- Cushner FD, Morwessel RM. Myositis ossificanstraumatica. OrthopRev 21 (1992): 1319-1326.
- Hait G, Boswick JA Jr, Stone NH. Heterotopic bone formationsecondary to trauma (myositisossificans traumatica). J Trauma 10 (1970): 405-411.
- Onen MR, Varol E, Tosun MI, Naderi S. Nontraumatic Myositis Ossificans as an Uncommon Cause of Scoliosis: Case Report and Review of the Literature. World Neurosurg 123 (2019): 208-211.
- Hanquinet S, Ngo L, Anooshiravani M, et al. Magnetic resonance imaging helps in the early diagnosis of myositis ossificans in children. PediatrSurgInt 15 (1999): 287-289.
- Akgun I, Erdogan F, Aydingoz O, et al. Myositis ossificans in early childhood: case report. Arthroscopy 14 (1998): 522-526.
- Russo R, Hughes M, Manolios N. Biopsy diagnosis of early myositis ossificans without radiologic evidence of calcification: success of early surgical resection. J ClinRheumatol 16 (2010): 385-387
- Barwad A, Banik T, Gorsi U, et al. Fine needle aspiration cytology of myositis ossificans. DiagnCytopathol 39 (2011): 432-434.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 75.63%
Acceptance Rate: 75.63%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
