Localized Disseminated Tuberculosis in A 3 Year’s Old Bangladeshi Boy: A Case Study
Article Information
Md. Jahedul Islam1*, Saika Farook2, Md. Enamul Karim3, Dilruba Yeasmin4, Mohammad Monirul Islam5, Prodip Kumar Sarkar6
1MD (Chest Diseases) Lecturer, Abdul Malek Ukil Medical College, Noakhali, Bangladesh
2Assistant Professor of Microbiology, Ibrahim Medical College (BIRDEM), Dhaka, Bangladesh
3Assistant Professor of Dermatology, Abdul Malek Ukil Medical College, Noakhali, Bangladesh
4MD (Chest Diseases), Assistant Registrar, National Institute of Diseases of the Chest and Hospital (NIDCH), Mohakhali, Dhaka, Bangladesh
5MD (Chest Diseases), Medical Officer, National Institute of Diseases of the Chest and Hospital (NIDCH), Mohakhali, Dhaka, Bangladesh
6Junior Consultant, Medicine, Kamrangirchar 31 Beded Hospital, Dhaka, Bangladesh
*Corresponding Author: Md Jahedul Islam, MD (Chest Diseases) Lecturer, Abdul Malek Ukil Medical College, Noakhali, Bangladesh.
Received: 01 October 2023; Accepted: 10 October 2023; Published: 29 February 2024
Citation: Md. Jahedul Islam, Saika Farook, Md. Enamul Karim, Dilruba Yeasmin, Mohammad Monirul Islam, Prodip Kumar Sarkar. Localized Disseminated Tuberculosis in A 3 Year’s Old Bangladeshi Boy: A Case Study. Archives of Clinical and Medical Case Report. 8 (2024): 30-35.
View / Download Pdf Share at FacebookAbstract
Introduction and importance: An uncommon clinical variant of TB infection known as localized disseminated tuberculosis exclusively manifests as hepatic injury-related signs and symptoms with little to no extrahepatic involvement. It typically manifests as a generalized syndrome with systemic symptoms, which can occasionally create a diagnostic conundrum. It can be exceedingly challenging to make a conclusive diagnosis and calls for a high index of suspicion.
Case presentation: Male Three-year-old patient was taken to the medical department because of a weeping visible lump in the disseminated TB area. Physical examination revealed nothing unusual, save for a bad overall state and hepatosplenomegaly-related discomfort. Parents say that nothing has changed over time. Yet after two weeks, the situation started to shift.
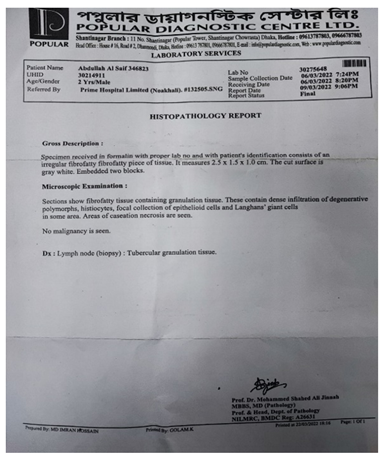
Clinical Discussion: The specimen that was received in formalin with the correct lab number and the patient's identification is made up of an atypical fibrofatty piece of tissue. It is 2.5*1.5*1.0 cm in size. the gray-white sliced surface was discovered. incorporated two blocks. An inspection under a microscope revealed fibrofatty tissue that included granulation tissue. They have a significant infiltration of Lamghan's giant cells, epithelioid lesions, histiocysts, and degenerative polymorphs in certain regions.
Conclusion: Atypical clinical symptoms are typically linked to tuberculosis. To confirm a diagnosis, particularly in cases of extrapulmonary TB, imaging evaluation along with histological characteristics, a high index of clinical suspicion, and improvement with antibacilar therapy are required.
Keywords
Disseminated Tuberculosis; Epithelioid Lesions; Histiocysts; Antibacilar Therapy
Disseminated Tuberculosis articles; Epithelioid Lesions articles; Histiocysts articles; Antibacilar Therapy articles
Article Details
Introduction
Even as we reach the next millennium, tuberculosis-one of the oldest illnesses known to mankind remains a significant issue. It continues to be the greatest cause of infectious illness mortality globally [1]. There is concrete proof that a worldwide pandemic [2] exists, and it has far from being completely eliminated. The emergence of multidrug resistant strains of Mycobacterium tuberculosis, migration of people from areas of high prevalence to areas of low endemicity, unfavorable social conditions, and ineffective public health surveillance programs are just a few of the factors contributing to the resurgence of tuberculosis. About 10% of TB cases are extrapulmonary, and cutaneous tuberculosis accounts for a very tiny part of these cases [3]. Children, whose immune systems are often underdeveloped and whose medicine compliance is typically poor, experience all of the aforementioned issues in greater detail. In India, 10%-15% of all fatalities in children under the age of 15 are thought to be related to tuberculosis [4]. Although though cutaneous TB only accounts for a small share of the tuberculosis cases in these kids, it is only reasonable that its prevalence has been rising accordingly. It is remarkable that there is so little research on children cutaneous TB given the complicating issues. Given that Mycobacterium TB (M. tuberculosis) was found in specimens taken from two non-contiguous organs, namely the lungs and the calcaneus, the patient in the case report had disseminated tuberculosis [5], by definition. When m. tuberculosis is isolated from blood, bone marrow, or specimens from two or more non-contiguous organs in a single patient, tuberculosis is said to have spread [6]. This concept has to take into account the molecular identification of M. tuberculosis in the current era of molecular diagnostics. Given that sufficient numbers of CD4 and CD8 T lymphocytes are needed to mount a host defense (via interferon gamma production) against M. tuberculosis infection [7] and in light of the observation that, even among subjects who do not have human immunodeficiency virus (HIV) coinfection, those with disseminated disease (military or localization in more than one location) were more likely to have the disease. Lymphocytopenia may have been a 4 Moreover, posttreatment CD4 levels in the study's disseminated illness remained considerably (P14 0.005) lower than comparable posttreatment cell counts in the study's localized disease [8]. Like in many high-burden nations, [9-10] Bangladesh has a shockingly low rate of pediatric tuberculosis (TB) detection. For children aged 0 to 14 years, the Bangladesh National Tuberculosis Programme (BNTP) reported a TB incidence of 9 per 100 000 [11]. Among of the more than 500 sub-districts in the nation, a 2008-2009 thorough study of two sub-districts reported a child TB prevalence of 52/100 000 children, which is over six times higher than official BNTP estimates. Adult TB prevalence in the same region was estimated to be 207/100,000 people, with children accounting for almost 20% of all cases identified. Considering these figures, it is predicted that the BNTP misses about 21 000 TB diagnoses in children each year [12]. According to our observations, the majority of children in Bangladesh who are diagnosed with TB are older than 8 years old, able to expectorate, or exhibit outward signs of the disease, including cervical lymphadenopathy or a gibbus [13-14]. This age and illness pro- le points to a serious underreporting of TB, particularly among the youngest and most fragile children, where it is most difficult to identify cases. We described a case report of a 3-year-old Bangladeshi kid who had localized, disseminated TB, and we emphasized the clinical illustration of this condition.
Case Report
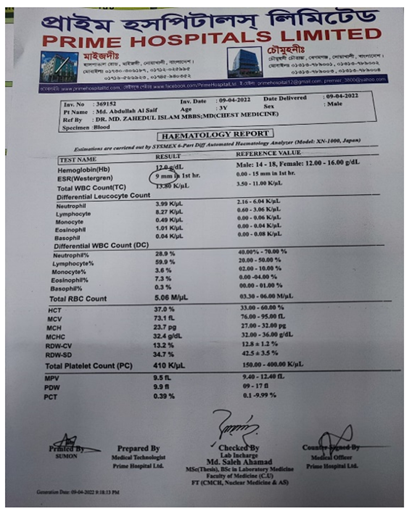
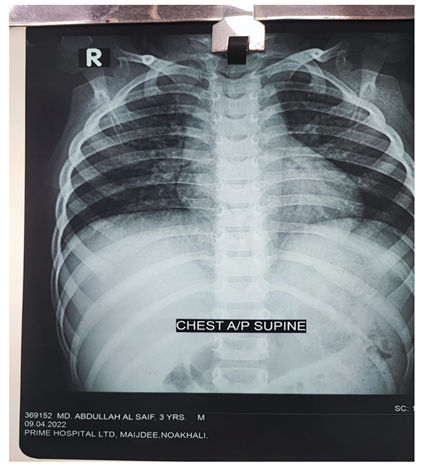
Male Patient, 3 years old was brought to the medicine department due to a visible mass in the disseminated tuberculosis region, which protruded with crying. Physical examination was unremarkable, except for a poor general condition and a tenderness associated with hepatosplenomegaly. Parents report no changes in size over time in a resting condition. But the size got changes after two weeks. Laboratory investigation showed that hemoglobin, 12.0g/dL; white blood cell count, 13.80 K/ul, with a shift to the left; platelet cell count, 410 K/ul; ESR 9mm in hr, Total RBC count 5.06 M/ul, HCT 37.0 %, Lymphocyte 8.27 K/ul, RDW-CV 13.2%, RDW-SD 34.7%. The histopathology report showed that Specimen received in formalin with proper lab no and with patient’s identification consists of an irregular fibrofatty piece of tissue. It measures 2.5X1.5X1.0 cm. The cut surface found as gray white. Embedded two blocks. Microscopic examination showed that fibro fatty tissue containing granulation tissue. These contain dense infiltration of degenerative polymorphs, histiocysts, focal collection of epithelioid cells and Lamghans giant cells in some areas. Areas of casearation nacrosis are seen. No maligency are seen. A computed tomographic (CT) scan of the thorax and abdomen revealed hepatomegaly, a thicker pericardium with symptoms of calcification, and a minor left pleural effusion. A chest X-ray indicated a distinct both side in bottom line effusion and there was now cardiomegaly. With a thicker pericardium and developing calcification mostly over the right heart and no obvious hemodynamic impairment, the echocardiography with color Doppler supported the diagnosis of constrictive pericarditis (CP).
Discussion
M. tuberculosis, which causes TB, is a chronic infectious illness that can affect any organ but primarily affects the lungs. The symptoms of TB vary depending on the underlying organ implicated in the disease. It typically manifests as a generalized constitutional illness with systemic symptoms, which can occasionally create a diagnostic conundrum. Less than 1% of all TB cases are hepatic, making it a rare [10] illness. 4 As a result of the lack of distinct clinical symptoms and imaging characteristics, the rate of clinical misdiagnosis is significant [11]. As in our case, the presenting symptoms were fever, night sweats, malaise, anorexia, weight loss, and abdominal discomfort, which are often vague and primarily constitutional in character. The primary symptom, hepatomegaly, is present in over 50% of patients [11] and is often discovered with an increase in liver tests. Nevertheless, these characteristics are not specific and can be seen in a variety of other illnesses and situations, including amyloidosis, echinococcosis, metastatic cancer, liver abscess, and granulomatous disorders with other etiologies. [12] Alkaline phosphatase and gamma glutamyl-transpeptidase levels are occasionally noticeably high, although serum aminotransferases and bilirubin levels might be modestly elevated or normal. [14] In some series, abnormal prothrombin times have frequently been discovered. Anemia, leukocytosis, and elevated erythrocyte sedimentation rates are typical non-specific test abnormalities. [16]. In our case study, all these laboratory abnormalities were seen. As the majority of granulomas are often found close to the portal system and liver function is only mildly perturbed, most patients have relatively moderate symptoms or are asymptomatic [17]. In disseminated TB autopsy series, liver involvement was discovered in 80-100% of the patients [18]. There were no indications of pulmonary illness in our patient. The emergence of a distinctive pleuritic discomfort and a tiny left pleural effusion, however, suggested this was another location of the illness. After lymph node involvement, pleural tuberculosis is the second most common extrapulmonary TB location [13]. Although the rupture of a subpleural caseous focus inside the lung into the pleural space is assumed to be the cause of pleural TB infection, it is possible that it occasionally results from hematogenous spread or contamination from nearby infected lymph nodes [13]. Since additional illnesses might be linked to a positive reaction, the tuberculin skin test is of limited utility as a diagnostic tool. It can also come back negative, especially in individuals with extrapulmonary TB [5]. T-cells that are specific for the M. tuberculosis antigen are discovered using more precise interferon gamma release assays (IGRAs) [5] When used in conjunction with strong clinical suspicion, radiography, and other medical and diagnostic assessments indicative of TB illness, this indirect test for tuberculosis infection-including infection leading to active disease-is authorized and of substantial value [14]. Sometimes the clinical diagnosis of TB is only verified after a patient has fully recovered as a result of antitubercular treatment [5]. In addition to the presence of epithelioid granulomas in the liver biopsy, pleural effusion, and signs of constrictive pericarditis on CT and echocardiography, the patient's low-grade fever, loss of appetite, hepatomegaly, and laboratory data that indicate a chronic inflammatory or infectious process all pointed toward tuberculosis as the primary diagnosis. Non-Hodgkin lymphoma was not suspected in a patient with systemic involvement because there was no lymphadenopathy and no aberrant blood morphology.
Conclusion
Extrapulmonary tuberculosis lacks the traditional clinical signs and imaging diagnostic, making it simple to make a false diagnosis and postpone treatment. The epithelioid granuloma with central caseating necrosis is the distinguishing feature of disseminated and extrapulmonary TB histopathology, and the diagnosis is made based on the discovery of acid-fast bacilli in a smear or culture and/or the presence of caseous granulomas in a tissue specimen. Yet, TB bacilli are hardly ever seen. The diagnosis of this entity, which is easily controlled medically but can be fatal if untreated, requires a high level of clinical suspicion.
Abbreviations
None
Conflicts of interest
None.
Sources of funding
Non-declared
Ethical approval
Hospital exempts ethics approval for reported cases
Consent Written
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Authorship contribution statement
All authors equally contributed to the analysis and writing of the manuscript.
Research registration
Not applicable.
Acknowledgement
None
Provenance and peer review
Not commissioned, externally peer-reviewed.
References
- Albrecht H. (n.d.). Bacterial and miscellaneous infections of the liver. Zakim and Boyer’s hepatology. A textbook of liver disease (2017): 656-670.
- Ayaslioglu E, Basar H, Duruyurek N, et al. Disseminated tuberculosis with lymphatic, splenic and scrotal abscesses: a case report. Cases Journal 2 (2009): 6995.
- Essop AR, Posen JA, Hodkinson JH, et al. Tuberculous hepatitis: a clinic review of 96 cases. Q J Med 53 (1984): 465-477.
- Fanning A. Tuberculosis: 6. Extrapulmonary disease. Journal de l’Association Medicale Canadienne. Canadian Medical Association Journal 160 (1999): 1597-1603.
- Ferrari TCA, Couto CM, Vilaça TS, et al. Localized hepatic tuberculosis presenting as fever of unknown origin. The Brazilian Journal of Infectious Diseases: An Official Publication of the Brazilian Society of Infectious Diseases 10 (2006): 364-367.
- Golden MP, Vikram HR. Extrapulmonary tuberculosis: an overview. American Family Physician 72 (2005): 1761-1768.
- Liao JR, Zhang D, Wu XL. Pulmonary tuberculosis combined with hepatic tuberculosis: a case report and literature review: Pulmonary and hepatic tuberculosis. The Clinical Respiratory Journal 9 (2015): 501-505.
- Maisch B, Seferovic PM, Ristic AD, et al. Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology. European Heart Journal 25 (2004): 587-610.
- Martinez L, Cords O, Liu Q, et al. Infant BCG vaccination and risk of pulmonary and extrapulmonary tuberculosis throughout the life course: a systematic review and individual participant data meta-analysis. The Lancet. Global Health 10 (2022): e1307-e1316.
- Mazurek GH, Jereb J, Vernon A, et al. Updated guidelines for using Interferon Gamma Release Assays to detect Mycobacterium tuberculosis infection - United States, 2010. Recommendations and Reports: Morbidity and Mortality Weekly Report 59 (2010): 1-25.
- Mert A, Ozaras R, Tabak F, et al. Localized hepatic tuberculosis. European Journal of Internal Medicine, 14 (2003): 511-512.
- Sabharwal BD, Malhotra N, Garg R, et al. Granulomatous hepatitis: a retrospective review. Indian J Pathol Microbiol 38 (1995): 413-416.
- Salama HM, Abdel-Wahab MF, Farid Z. Hepatobiliary disorders presenting as fever of unknown origin in Cairo, Egypt: the role of diagnostic ultrasonography. The Journal of Tropical Medicine and Hygiene 91 (1988): 147-149.
- Sharma SK, Tripathi M. Addison’s disease due to histoplasmosis of bilateral adrenal glands in a previously treated extrapulmonary tuberculosis case. The Indian Journal of Medical Research 152 (2020): S1-S3.
- Sharma S, Shachita, Bhardwaj P. Extrapulmonary Tuberculosis manifests as Middle Ear Tuberculosis: A rare case report from secondary health care center at Sub-Himalayan region. International Journal of Science and Healthcare Research 7 (2022): 9-11.
- Singh S, Jain P, Aggarwal G, et al. Primary hepatic tuberculosis: a rare but fatal clinical entity if undiagnosed. Asian Pacific Journal of Tropical Medicine 5 (2012): 498-499.
- Tritou I, Prassopoulos P, Daskalogiannaki M, et al. Miliary hepatic tuberculosis not associated with splenic or lung involvement. A case report. Acta Radiologica (Stockholm, Sweden: 1987) 41 (2000): 479-481.
- Wu Z, Wang W, Zhu Y, et al. Case report. Diagnosis and treatment of hepatic tuberculosis: report of five cases and review of literature. Int J Clin Exp 6 (2013): 845-850.



 Impact Factor: * 3.1
Impact Factor: * 3.1 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
