Nose Necrosis in Female Shocked Patient: Conservative Treatment with Heparin
Marco Stabile MD*, Luca Rosato MD and Valeria Navach MD
Plastic Surgery Unit Piacenza Hospital, Italy
*Corresponding Author: Marco Stabile, Head of Plastic Surgery Unit Piacenza Hospital, Italy
Received: 06 January 2023; Accepted: 07 February 2023; Published: 03 August 2023
Article Information
Citation: Marco Stabile, Luca Rosato, Valeria Navach. Nose Necrosis in Female Shocked Patient: Conservative Treatment with Heparin. Archives of Clinical and Medical Case Reports. 7 (2023): 335-337
View / Download Pdf Share at FacebookKeywords
Acute skin necrosis; Heparin; skin hypoperfusion
Skin Necrosis articles, Heparin, Female Shock articles, Topical Heparin articles, Skin conservative treatment with Heparin articles
Acute skin necrosis articles Acute skin necrosis Research articles Acute skin necrosis review articles Acute skin necrosis PubMed articles Acute skin necrosis PubMed Central articles Acute skin necrosis 2023 articles Acute skin necrosis 2024 articles Acute skin necrosis Scopus articles Acute skin necrosis impact factor journals Acute skin necrosis Scopus journals Acute skin necrosis PubMed journals Acute skin necrosis medical journals Acute skin necrosis free journals Acute skin necrosis best journals Acute skin necrosis top journals Acute skin necrosis free medical journals Acute skin necrosis famous journals Acute skin necrosis Google Scholar indexed journals Anesthesia articles Anesthesia Research articles Anesthesia review articles Anesthesia PubMed articles Anesthesia PubMed Central articles Anesthesia 2023 articles Anesthesia 2024 articles Anesthesia Scopus articles Anesthesia impact factor journals Anesthesia Scopus journals Anesthesia PubMed journals Anesthesia medical journals Anesthesia free journals Anesthesia best journals Anesthesia top journals Anesthesia free medical journals Anesthesia famous journals Anesthesia Google Scholar indexed journals necrosis articles necrosis Research articles necrosis review articles necrosis PubMed articles necrosis PubMed Central articles necrosis 2023 articles necrosis 2024 articles necrosis Scopus articles necrosis impact factor journals necrosis Scopus journals necrosis PubMed journals necrosis medical journals necrosis free journals necrosis best journals necrosis top journals necrosis free medical journals necrosis famous journals necrosis Google Scholar indexed journals Heparin articles Heparin Research articles Heparin review articles Heparin PubMed articles Heparin PubMed Central articles Heparin 2023 articles Heparin 2024 articles Heparin Scopus articles Heparin impact factor journals Heparin Scopus journals Heparin PubMed journals Heparin medical journals Heparin free journals Heparin best journals Heparin top journals Heparin free medical journals Heparin famous journals Heparin Google Scholar indexed journals Ultrasound articles Ultrasound Research articles Ultrasound review articles Ultrasound PubMed articles Ultrasound PubMed Central articles Ultrasound 2023 articles Ultrasound 2024 articles Ultrasound Scopus articles Ultrasound impact factor journals Ultrasound Scopus journals Ultrasound PubMed journals Ultrasound medical journals Ultrasound free journals Ultrasound best journals Ultrasound top journals Ultrasound free medical journals Ultrasound famous journals Ultrasound Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals Seminoma articles Seminoma Research articles Seminoma review articles Seminoma PubMed articles Seminoma PubMed Central articles Seminoma 2023 articles Seminoma 2024 articles Seminoma Scopus articles Seminoma impact factor journals Seminoma Scopus journals Seminoma PubMed journals Seminoma medical journals Seminoma free journals Seminoma best journals Seminoma top journals Seminoma free medical journals Seminoma famous journals Seminoma Google Scholar indexed journals Vitrectomy articles Vitrectomy Research articles Vitrectomy review articles Vitrectomy PubMed articles Vitrectomy PubMed Central articles Vitrectomy 2023 articles Vitrectomy 2024 articles Vitrectomy Scopus articles Vitrectomy impact factor journals Vitrectomy Scopus journals Vitrectomy PubMed journals Vitrectomy medical journals Vitrectomy free journals Vitrectomy best journals Vitrectomy top journals Vitrectomy free medical journals Vitrectomy famous journals Vitrectomy Google Scholar indexed journals skin hypoperfusion articles skin hypoperfusion Research articles skin hypoperfusion review articles skin hypoperfusion PubMed articles skin hypoperfusion PubMed Central articles skin hypoperfusion 2023 articles skin hypoperfusion 2024 articles skin hypoperfusion Scopus articles skin hypoperfusion impact factor journals skin hypoperfusion Scopus journals skin hypoperfusion PubMed journals skin hypoperfusion medical journals skin hypoperfusion free journals skin hypoperfusion best journals skin hypoperfusion top journals skin hypoperfusion free medical journals skin hypoperfusion famous journals skin hypoperfusion Google Scholar indexed journals
Article Details
1. Introduction
Acute skin failure is an event in which skin and underlying tissue die due to hypoperfusion concurrent with a critical illness [1]. Usually skin hypoperfusion is a late symptom in a shock setting and it is present in patients with an advanced multiorgan failure (MOF) dysfunction. Acute skin damage is mainly present in feet and hands as consequence of distal hypoperfusion due to hypotension or microthrombotic events [2]. Face is less commonly affected. In some cases of purpura fulminas there is anyway an important face skin involvement. Purpura fulminans is usually associated with meningococcal sepsis, varicella, and pneumococcal infections and\or coagulation disorders [3-4]. We present the clinical case of a young woman occurring at our hospital with nose skin necrosis as first sing of shock setting.
2. Case History
A 38 years old woman presented at the Emergency Department in sleepy state, generalized malaise and fever unresponsive to paracetamol. The patient had marbling on the extremities and on the face. The anamnestic investigation did not reveal anything of clinical significance. After 24 hours, the clinical picture turned into septic shock with intravascular disseminated coagulation. Marbling of the extremities persisted and on the nose it progressed in partial necrosis. Clinical blood and cerebrospinal fluid samples tests were negative; anyway empiric therapy with vancomycin and meropenem was started. Renal and hepatic function resulted compromised. Blood support circle (noradrenaline and dopamine therapy) was administered for the first 3 days. Breathing support was necessary for 2 days, and then only occasionally oxygen support was requested. Subcutaneous therapy with enoxaparine was administered (4000 UI per day) until discharge. Single dose of Antithrombin III was given on third day. After 72 hours the patient quickly recovered. The clinical picture and the multiorgan failure state progressively improved and patient was transferred from intensive care to infective department. The specialist haematological consultation and all tests carried didn’t revealed pathologies of haematological branch.
Three days after recovery the plastic surgeon was called for the evaluation of facial injuries. The patients showed a full thickness necrosis of the skin of the tip of nose and faded marbling of the rest of the nose and cheeks (Figure 1). Conservative treatment was chosen and started with daily topic applications of "Epsodilave 250 UI / 5ml" (sodic heparin) and greasy gauze dressing. Two days after, the necrosis showed an improvement and it was limited to the more distal areas of the nose (Figure 2). The topical treatment continued for 18 days until the patient was discharged. No surgical or chemical debridement was carried out. Extremities marbling had a spontaneous regression. One month later, the patient came to control showing a complete remission and resolution without significant scarring (Figure 3).

Figure 1: Full thickness necrosis of the skin of the tip of nose and faded marbling of the rest of the nose and cheeks.

Figure 2: The necrosis showed an improvement and limited to the more distal areas of the nose.
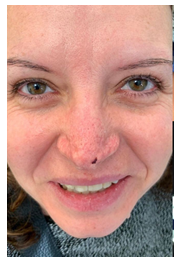
Figure 3: Complete remission and resolution without significant scarring.
3. Discussion
Acute skin necrosis due to severe and prolonged hypotension can be present in advanced shock settings. Usually extremities are affected, because of their distinctive vascular pattern. These signs become evident later respect to other shock typical symptoms [5]. In our case, skin failure was an early expression of critical illness status. Later the patient got worse in a MOF status, with compromised renal and hepatic function. The unique localization of the nose skin necrosis addressed clinicians towards a purpura diagnosis. All examination (blood coagulation pattern, absence of meningococcal infection in blood and cerebrospinal fluid) contradicted this hypothesis. The hematologist also excluded any disease of hiss clinical branch. We finally concluded the damage at nose skin was due solely to hypoperfusion. Nose has a rich vascularization from facial artery in the lower part and from angular branch in the upper part. All these branches anastomose at the lateral sides. Nasal tip lacks anyway of a strong vascularization and it is more prone to hypoperfusion.
There are not standardized treatments for acute skin failure, maybe also because in a life threatening setting, treatment of skin lesions is not considered relevant. Minor lesions can regress after reset of blood circle, but established skin necrosis needs specific treatment. The nasal soft tissue envelope is composed of fat, muscle, overlying superficial musculoaponeurotic system, and skin. The caudal half of the nose contains also a higher density of sebaceous glands [6]. Surgical debridement in case of nose skin necrosis is commonly discouraged. The deeper sebaceous layers especially at the tip, have an important regenerative capacity, so conservative procedures are preferred. Many topical treatments are described in literature. Use of vasodilators such as ointment with nitroglycerine and systemic or topical treatment with pentoxifylline or prostaglandin E1 were used. Hyperbaric treatment is also described by some authors. The cost and the management of these treatments are not often suitable for critical illness patients. In our experience, we had good results in the topic use of heparin on burns and skin necrosis, that’s why we routinely use it for cutaneous lesions that need conservative treatment.
Ng in his review of literature underlines that topic treatment with gel containing heparin improves or positively alter the microcirculation in normal skin at both deep and superficial capillary layers [7]. Also patients with microangiopathy and have a significant improvement after treatment with topical use of heparin. Heparin molecule is a long glycosamminoglicane. Apart its role in coagulation process, it has also anti-inflammatory property. For this reason heparin and its derivate are also used in the treatment of asthma, inflammatory bowel disease, cardiopulmonary bypass, and cataract surgery [8]. Many mechanisms are involved in the anti-inflammatory effect. Levels of citocytokines after heparin administration are decreased (IL 6, IL 8, TNF) and heparin also inhibits adhesion of leukocytes and neutrophils to endothelial cells.
The topical use of heparin on damaged skin has been long described in the treatment of burns by Saliba with excellent results in terms of healing; scarring and pain control [9-10]. At our advice the use of topical heparin is a valid treatment in case of skin damage due to vascular impairment. We recommend trying this before surgical debridement.
References
- Langemo DK, Brown G. Skin fails too: acute, chronic, and end-stage skin failure. Adv Skin Wound Care 19 (2006): 206-211.
- Dalgleish L, Campbell J, Finlayson K, et al. Acute Skin Failure in the Critically Ill Adult Population: A Systematic Review. Adv Skin Wound Care 33 (2020): 76-83.
- Moon SM, Hong YS, Lee DS, et al. Purpura fulminans on the nose with septic abortion. Intensive Care Med 41 (2015): 1122.
- Walsh LF, Sherbuk JE, Wispelwey B. Pneumococcal induced thrombotic thrombocytopenic purpura with features of purpura fulminans. BMJ Case Rep 14 (2021): e235580.
- Warkentin TE, Ning S. Symmetrical peripheral gangrene in critical illness. Transfus Apher Sci 60 (2021): 103094.
- Kerolus JL, Nassif PS. Treatment Protocol for Compromised Nasal Skin. Facial Plast Surg Clin North Am 27 (2019): 505-511.
- Ng L, Monagle K, Monagle P, et al. Topical use of antithrombotics: review of literature..Thromb Res 135 (2015): 575-581.
- Mousavi S, Moradi M, Khorshidahmad T, et al. Anti-Inflammatory Effects of Heparin and Its Derivatives: A Systematic Review. Adv Pharmacol Sci 2015 (2015): 507151.
- Heparin in the treatment of burns: a review. Saliba MJ Jr.Burns 27 (2001): 349-358.
- Venakatachalapathy TS, Mohan Kumar S, Saliba MJ. A comparative study of burns treated with topical heparin and without heparin. Ann Burns Fire Disasters 20 (2007):189-198.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 75.63%
Acceptance Rate: 75.63%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
