Pediatric Recurrent Vesicular Palmoplantar Dermatitis Presenting with Pyrexia: A Case Report
Nayla Al Khalifa1*, Mazen Raees2, Salman Al Khalifa3, Eman Al Juffairi4
1Resident, Dermatology, Internal Medicine Department, King Hamad University Hospital, Busaiteen, Kingdom of Bahrain
2Consultant in Dermatology and Venereology, Internal Medicine Department, King Hamad University Hospital, Busaiteen, Kingdom of Bahrain
3Consultant Pediatrician and Pulmonologist, Pediatrics Department, King Hamad University Hospital, Busaiteen, Kingdom of Bahrain
4Consultant in Pathology, Pathology Department, King Hamad University Hospital, Busaiteen, Kingdom of Bahrain
*Corresponding Author: Nayla Al Khalifa, Resident, Dermatology, Internal Medicine Department, King Hamad University Hospital, Busaiteen, Kingdom of Bahrain
Received: 12 December 2023; Accepted: 16 January 2024; Published: 23 January 2024
Article Information
Citation: Nayla Al Khalifa, Mazen Raees, Salman Al Khalifa, Eman Al Juffairi. Pediatric Recurrent Vesicular Palmoplantar Dermatitis Presenting with Pyrexia: A Case Report. Archives of Clinical and Medical Case Reports 8 (2024): 13-15.
View / Download Pdf Share at FacebookAbstract
Background: Recurrent palmoplantar dermatitis is a a subtype of chronic hand eczema, presenting with deep-seated palmoplantar vesicles or bullae. Although demographics of recurrent palmoplantar dermatitis in the pediatric age group is obscure, the disorder was found to commonly affect children. Moreover, no standardized global diagnostic and treatment guidelines have been established yet.
Case presentation: In this case report, we present a 5-year-old male patient, known case of nummular dermatitis, presenting with severe palmoplantar bullae and fever.
Conclusions: To date, this is the first case presentation demonstrating a possible viral trigger in pediatric recurrent palmoplantar dermatitis. Further large-scale studies can potentially prove such etiology.
Keywords
<p>Vesicular; Palmoplantar; Dermatitis; Bullae; Pemphigoid</p>
Article Details
List of Abbreviations:
Recurrent Vesicular Palmoplantar Dermatitis (RVPD); Dyshidrotic Eczema (DE); Chronic Hand Eczema (CHE); Pediatric CHE (P-CHE); Atopic Dermatitis (AD); Erythrocyte Sedimentation Rate (ESR); Bullous Pemphigoid (BP); Immunoglobulin (Ig); Periodic Acid-Schiff (PAS); Topical Corticosteroids (TCS); Psoralen Plus Ultraviolet-A Radiation (PUVA).
1. Introduction
Recurrent Vesicular Palmoplantar Dermatitis (RVPD), previously known as dyshidrotic eczema (DE) or pompholyx [1,2], is a disorder categorized as a subtype of chronic hand eczema (CHE) [3]. Although demographics of RVPD in children is obscure [1,2,3], more than 1 in 20 children are affected by pediatric CHE (P-CHE) in the United States and Canada [3]. RVPD typically presents with symmetrical deep-seated vesicles or bullae on the lateral fingers, palms, or soles [1,2, 4, 5], usually preceded by itching or paresthesia [2,5]. First described by Fox as a disorder of sweat dysfunction [1], etiology remains mostly idiopathic [1,2,5]. Triggers include hyperhidrosis, dermatophytosis, and contact allergens [1, 2,5]. More importantly, most P-CHE and RVPD were associated with atopic dermatitis (AD) [3,4,5]. RVPD is a clinical diagnosis [1], and histopathology may confirm the disease [2, 4]. Mycological exam, patch testing, and immunofluorescence can rule out other differential diagnoses [1,2,3,6]. RVPD is generally successful to treatment, with treatment options ranging from topical corticosteroids to systemic therapies [3-5].
Because there is no established consensus on RVPD in children [1,2,3], this case aims to demonstrate a possible viral trigger. To date, this is the first case presentation demonstrating RVPD presenting with tense bullae in a febrile, 5-year-old child with nummular dermatitis.
2. Case Presentation
A 5- year-old male, known case of nummular dermatitis, was admitted with fever and tender palmoplantar blisters, which were preceded by erythema and pruritus (Figure 1). On examination, the patient had a fever, measuring 38.6 degrees Celsius, tense palmoplantar bullae, and eczematous discoid patches on the extremities. Routine blood investigations were normal apart from a high eosinophil absolute count of 1.03 x10 9/l and high erythrocyte sedimentation rate (ESR) of 56. Bullous pemphigoid (BP) 180 and 230 immunoglobulin (Ig) G antibodies were negative. Ig A, E, D, G, and M were normal. Throat swab, urine culture, and serology for Coxackie and Enterovirus were normal. Skin biopsy confirmed RVPD (Figure 3 A & B). Sections demonstrated subepidermal bulla filled with scant mixed inflammatory cells, with the roof showing squamous epithelium exhibiting parakeratosis, patchy loss of granular layer and rare dyskeratotic cells. Periodic acid-Schiff (PAS) histochemical stain did not show fungus, and immunofluorescence studies for IgA, IgG, IgM, C1q, C3 and fibrinogen were all negative. No basement membrane or inter-cellular staining was noted.
The patient was initiated on a mixture of Betamethasone Dipropionate and Fusidic acid cream, which resolved the lesions completely within two weeks (Figure 2).

Figure 1: Symmetrical palmar bullae on non-erythematous base

Figure 2: Resolution of bullae
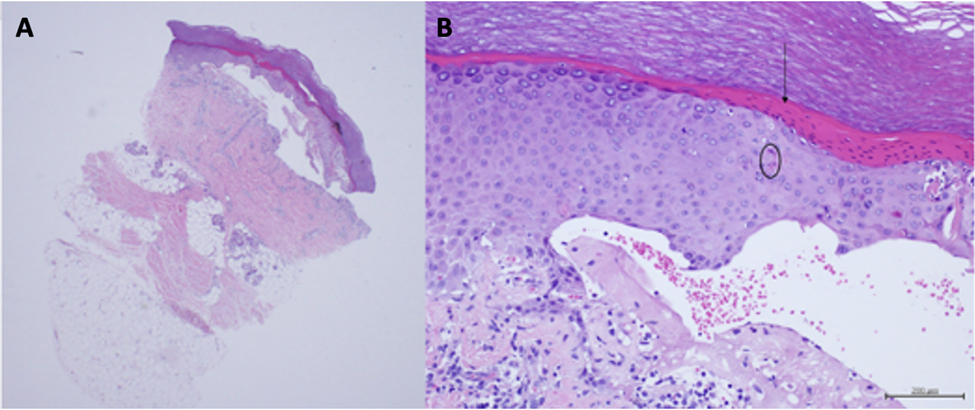
Figure 3 A & B: Skin biopsy shows subepidermal bulla with hyperkeratosis and parakeratosis [arrow], dyskeratosis (circle) and absent granular layer. (Hematoxylin & Eosin stain, A: x20 magnification, B: x200 magnification).
3. Discussion
Since there is no established consensus on RVPD in pediatric patients, and data on clinical phenotype, epidemiology and management guidelines remain variable [1,2,3], this case serves an opportunity to clarify that RVPD may be triggered by a virus. Self-limited or recurrent severe eruption of symmetrical palmoplantar bullae on non-erythematous base differentiated RVPD from dyshidrosiform eruptions, such as contact dermatitis, dermatophytosis, and drug eruptions [1, 2, 3, 5]. Moreover, the atopic status of our patient predisposed him to have RVPD, defined by his discoid eczematous patches. Hence, establishing atopic stigmas, such as eczematide-like patches, atopic family history, elevated serum IgE level or eosinophilia are clues to diagnosing RVPD, which according to a recent cross-sectional study, was associated with atopic dermatitis in 77.8% of patients [1].
Although Coxackie and Enterovirus viral serology were normal, RVPD could have been possibly triggered by a virus as confirmed by the high eosinophil count and high ESR. Furthermore, mycological exam and patch testing may be necessary to exclude dermatophytosis and contact allergy, respectively [2,3,5]. Because localized dyshidrotic bullous pemphigoid (BP) also presents with palmoplantar vesiculobullous lesions, direct immunofluorescence is necessary. Linear deposition of IgG at the dermo-epidermal junction is consistent with dyshidrotic BP [6].
Topical corticosteroids (TCS) remain the first line management for mild to moderate RVPD, and short course of oral prednisolone may be necessary [3,5]. Dupilumab yields complete clearance within four to six weeks in refractory RVPD [3,4]. Studies demonstrated successful outcomes with combination of Botulinum Toxin-A and TCS [5]. Alitretinoin and cyclosporine were discouraged due to premature epiphyseal closure and hypertension, respectively [3]. Complete remission was achieved with oral psoralen plus ultraviolet-A radiation (PUVA) as opposed to other radiotherapy modalities [5].
4. Conclusion
Despite no standardized phenotype, diagnosis, and management guidelines have been established [1,2,3], this case highlights the possibility of a viral trigger in RVPD. Atopy is highly associated with RVPD and can serve as a diagnostic clue when distinguishing RVPD.
Consent
The patient has given their written informed consent for the case and images to be published.
Clinical Message
Dr. Nayla Al Khalifa, Dr. Mazen Raees, Dr. Salman Al Khalifa, and Dr. Eman Al Juffairi aimed to demonstrate the possibility of a viral trigger in RVPD.
Competing Interests
The authors declare they have no competing interests.
Author’s Corner
Dr. Nayla Al Khalifa, Dr. Mazen Raees, Dr. Salman Al Khalifa, and Dr. Eman Al Juffairi are satisfied with this research publication.
Funding
This study has not been funded.
Data Availability Statement
All data underlying the results are available as part of the article and no additional source data are required.
Author Contributions
All authors have accepted responsibility for the entire content of this manuscript and approved its submission. Dr. Nayla Al Khalifa prepared the manuscript, whilst Dr. Mazen Raees and Dr. Salman Al Khalifa supervised the patient’s diagnosis, patient’s management and manuscript. Dr. Eman Al Juffairi provided the histopathology images with the appropriate description.
References
- Scotelaro-Alves HG, Fernandes NC, Ramos-E-Silva M. Clinical profile of recurrent vesicular palmoplantar dermatitis in children and adolescents. Clin Cosmet Investig Dermatol 12 (2019): 23-28.
- Mrudula S, Nandakishore T, Kongbam L, Valsalan B, Nischith V, et al. Recurrent vesicular palmoplantar dermatitis: a clinical study in children and adolescents. Int J Res Dermatol 9 (2023): 73-77.
- Haft MA, Park HH, Lee SS, Sprague JM, Paller AS, et al. Diagnosis and Management of Pediatric Chronic Hand Eczema: The PeDRA CACHES Survey. Pediatr Drugs 25 (2023): 459–466.
- Yali Li, Xiao J, Sun Yi, Fang H, Qiao J, et al. Quick Treatment of Very Severe Refractory Hand and Foot Eczema with Dupilumab: A Case Report and Literature Review. J Asthma Allergy 16 (2023): 1–8.
- Thyssen JP, Menné T. Acute and Recurrent Vesicular Hand Dermatitis. Kanerva's Occupational Dermatology. Springer 1 (2012): 185-195.
- Surabhi D, Sahu P, Jain VK, et al. Dyshidrosiform pemphigoid localized on the hands in a child: a rare occurrence. An Bras Dermatol 92 (2017): 714-716.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 75.63%
Acceptance Rate: 75.63%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
