Renal Scintigraphy in Combination with Intravenous Pyelogram for the Diagnosis of Nephroptosis
Jiaqiong Wang1*, Taylor Standiford2, Jessica Pryor3, Brian Chao3, Daniel D Eun3, Yi Li4, Maria Meinel1, Simindokht Dadparvar1, Jian Q Yu1
1Division of Nuclear Medicine, Department of Radiology, Temple University Hospital, Fox Chase Cancer Center, Philadelphia, USA
2Abdominal Imaging Section, Department of Diagnostic Radiology, University of Pennsylvania, Philadelphia, USA
3Department of Urology, Temple University Hospital, Philadelphia, USA
4Division of Nuclear Medicine and Division of Body Imaging, Department of Radiology, Fox Chase Cancer Center, Philadelphia, USA
*Corresponding Author: Jiaqiong Wang, MD, PhD, Assistant Professor, Division of Nuclear Medicine, Department of Radiology, Temple University Hospital, Fox Chase Cancer Center, 3401 N Broad St, Philadelphia, PA 19140, USA
Received: 25 February 2024; Accepted: 08 March 2024; Published: 14 March 2024
Article Information
Citation:
Jiaqiong Wang, Taylor Standiford, Jessica Pryor, Brian Chao, Daniel D Eun, Yi Li, Maria Meinel, Simindokht Dadparvar, Jian Q Yu. Renal Scintigraphy in Combination with Intravenous Pyelogram for the Diagnosis of Nephroptosis. Archives of Clinical and Medical Case Reports. 8 (2024): 42-51.
View / Download Pdf Share at FacebookAbstract
Nephroptosis is defined as kidney descent more than 2 vertebral bodies (or >5 cm) during a position change from supine to upright. The current gold diagnostic standard is visual descent seen on intravenous pyelograms (IVP), which is limited to anatomical change. Renal scintigraphy would complement IVP to make the diagnosis of nephroptosis, and facilitate the evaluation of renal function. We report a series of 5 patients suspicious of nephroptosis who were examined by both IVP and renal scintigraphy with Tc-99m diethylenetriaminepentaacetic acid (Tc-99m DTPA) in the supine and upright positions. Renal scintigraphy was performed with a Co-57 source marker to locate the anterior iliac crest. Three cases were consistent with nephroptosis on IVP, four cases were consistent with nephroptosis on renogram. One case was consistent with nephroptosis on renogram but missed on IVP. One case was negative on both IVP and renogram. Some nephroptosis cases demonstrated decrease in calculated split renal function in the upright position. Renal scintigraphy is a valuable tool in the evaluation of nephroptosis. Renal scintigraphy can provide location information similar to IVP, and complementary functional information, which may aid urologists in confirming the diagnosis and selecting patients for nephropexy.
Keywords
<p>Nephroptosis; Intravenous pyelogram; Renal scintigraphy; Glomerular filtration rate; Renal function</p>
Article Details
1. Introduction
Nephroptosis, also known as floating or wandering kidney, is an uncommon condition in which one or both kidneys drop below their correct position in the abdomen when the patient stands up. Most patients are asymptomatic or with mild symptoms. Some patients present with abdominal pain and/or flank pain after standing for greater than 20-30 minutes, and the pain typically decreases when lying down [1]. Other symptoms include nausea and vomiting, hematuria, and orthostatic hypertention [2, 3]. The condition has been traditionally defined as kidney descent of greater than two vertebral bodies (or >5 cm) during a position change from supine to upright. Current treatment for patients with severe symptoms includes robotic or laparoscopic nephropexy to fixate the kidney in its cranial-most, undescended position [4, 5]. This surgical procedure is based upon the correct diagnosis of nephroptosis and appropriate selection of patients. However, it is challenging to make the correct diagnosis of nephroptosis because it usually appears normal on the conventional imaging utilizing CT urography or retrograde pyelography when the patient is lying in the supine position. Currently, the gold standard for the diagnosis of nephroptosis is visual descent seen on intravenous pyelograms (IVP) after a position change from supine to upright [6, 7]. However, IVP is limited to delineating only the anatomical change. Other imaging modalities such as color Doppler imaging is useful to assess change of renal blood flow in case of nephroptosis [8], but it cannot evaluate renal function. Nuclear renal scintigraphy with Technetium-99m mercaptoacetyltriglycine (Tc-99m MAG3) and Tc-99m DTPA can be utilized to evaluate renal location, size, blood flow, renal function, as well as to assess urinary obstruction if present [9, 10]. In the current study, we evaluated patients with symptoms suspicious of nephroptosis with both IVP and nuclear renal scintigraphy with Tc-99m DTPA. We hypothesize that nuclear renal scintigraphy would complement IVP to better establish a diagnosis of nephroptosis, facilitate pre-operative evaluation of renal blood flow and function, and guide surgical decision making.
2. Methods
Five patients with symptoms suspicious for nephroptosis were evaluated by both IVP and nuclear renal scintigraphy with Tc-99m DTPA between January 2019 and December 2022. For each patient, IVP was performed at the anterior-posterior projection after the intravenous injection of 100 ml Omnipaque 350, supine radiographs were obtained after initial intravenous contrast excretion, and subsequently upright radiographs were obtained after prolonged standing for 20-30 minutes. Nuclear renal scintigraphy with Tc-99m DTPA was performed in the supine and upright positions sequentially with the camera close to the patient’s back. First, in the supine position, routine nuclear renogram was performed with intravenous bolus administration of 10 mCi Tc-99m DTPA, a radionuclide angiogram of perfusion to the kidneys was acquired, then dynamic images of the kidneys were obtained over 30 minutes to evaluate renal cortical uptake and excretion. These data were used to analyze renal flow and function, and additional post void images were acquired. The time interval was approximately 40-180 minutes (average 90 minutes) between the renal scintigraphy in the supine and upright positions. In the upright position, nuclear renal scintigraphy was repeated with 20 mCi of Tc-99m DTPA using the same image acquisition protocol to evaluate the difference in the renal location and function. A Co-57 source marker was utilized to mark the anterior iliac crest throughout the duration of the scans and to maintain consistency of the scan positions. Glomerular filtration rate (GFR) was calculated using Gates’ method for renal scintigraphy in supine and upright positions [11]. Split renal functions were calculated based on renal radioactivity on renal scintigraphy 2-3 minutes post injection of radiotracer [12]. The study protocol was approved by the institutional review board of the university.
3. Overall Results
Five patients presented to our institution with concern for nephroptosis between January 2019 and December 2022. These patients underwent evaluation with both nuclear renal scintigraphy with Tc-99m DTPA and IVP in the supine and upright positions. Three cases were consistent with the diagnosis of nephroptosis on IVP, four cases were consistent with the diagnosis of nephroptosis on renal scintigraphy. One case was consistent with the diagnosis of nephroptosis on the renal scintigraphy but missed on IVP. One case was negative for nephroptosis on both IVP and renal scintigraphy.
Brief Summary of Cases
Case 1
Case 1 was a 44 year-old female who presented with chronic left flank pain and new onset right flank pain. She had a prior history of left gonadal vein embolization for pelvic congestion with partial relief of her left flank pain. She stated that her right flank pain was absent when she woke up in the morning, but worsened after prolonged sitting or standing. IVP (Figure 1A and 1B) and renogram (Figure 1C and 1D) both demonstrated significant descent of the right kidney in the upright position, consistent with right nephroptosis. IVP initial supine radiographs after intravenous contrast excretion showed the right kidney within the mid abdomen, with no evidence of hydronephrosis (Figure 1A). Contrast excretion was identified within the renal calyces and pelvis, proximal mid and distal ureters in various segments. After prolonged standing, the upright imaging showed that the right kidney descended approximately 10 cm into the right pelvis (Figure 1B). With descent, there was extensive tortuosity and kinking of the right proximal and mid ureter (Figure 1B). Renal scintigraphy with Tc-99m DTPA was performed with approximately 40 minutes between the supine position (Figure 1C) and the upright positon, and demonstrated descent and malrotation of the right kidney in the upright position (Figure 1D). There was normal blood flow to bilateral kidney. In the supine position, the estimated total glomerular filtration rate (GFR) was 108 ml/min, the split renal function was 48.1% on the right and 51.9% on the left. In the upright position, the estimated total GFR was 88 ml/min, the split renal function was 39.9% on the right and 60.1% on the left, suggestive of interval decreased function of the right kidney (Table 1). The decrease in the total GFR was mainly due to decreased right renal function.
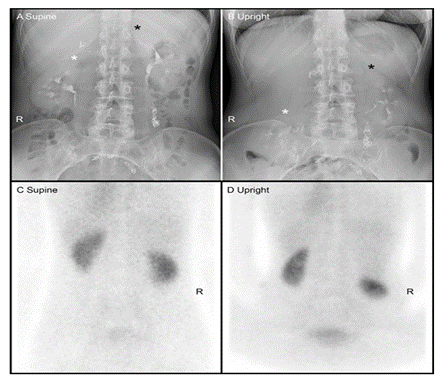
Figure 1: Intravenous pyelogram (IVP) and renal scintigraphy of case 1. IVP initial supine radiographs showed the right kidney within the mid abdomen, the superior border of the right kidney (white * in A) was at the level of L2 superior endplate, with no evidence of hydronephrosis(A). Contrast excretion was observed within the renal calyces and pelvis, proximal mid and distal ureter in various segments. After prolonged standing, the upright imaging showed that the right kidney descended approximately 10 cm into the right pelvis, the superior border of the right kidney (white * in B) was at the L4 level. With descent, there was extensive tortuosity and kinking of the right proximal and mid ureter (B). Renal scintigraphy with Tc-99m DTPA was performed with approximately 40 minutes between the supine position (C) and the upright positon (D), and demonstrated descent and malrotation of the right kidney in the upright position (D).
Table 1: Renal split function of case 1 in the supine and upright positions.
|
Right |
Left |
|
|
Supine |
48.10% |
51.90% |
|
Upright |
39.90% |
60.10% |
Case 2
A 41 year- old male had a history of motor vehicle accident in 2018 and subsequently developed bilateral flank pain. The pain was ameliorated with lying down and worsened with standing up. Both IVP (Figure 2A and 2B) and renal scintigraphy (Figure 2C and 2D) failed to demonstrate supraphysiologic descent of either kidney in the upright position. Supine and prolonged standing radiographs (Figure 2A and 2B) did not show radiographic evidence of nephroptosis. Initial supine radiographs after intravenous contrast excretion demonstrated both kidneys at the expected physiological position (Figure 2A). With prolonged standing, there was descent of the right kidney into the lower abdomen by 2.8 cm and descent of the left kidney by 3.1 cm (Figure 2B). The patient did not report any pertinent symptoms in the supine position during the exam. Renal scintigraphy with Tc-99m DTPA was performed with approximately 180 minutes between the supine and upright positions (Figure 2C and 2D), and did not demonstrate supraphysiologic descent of either kidney in the upright position (Figure 2d). There was normal blood flow to the bilateral kidneys. In the supine position, the estimated total GFR was 130 ml/min, the split renal function was 43.2% on the right and 56.8% on the left. In the upright position, the estimated total GFR was 111ml/min, the split renal function was 49.3% on the right and 50.7% on the left, no significant change from the supine position (Table 2). With the exclusion of nephroptosis, the patient did not proceed to surgical fixation.
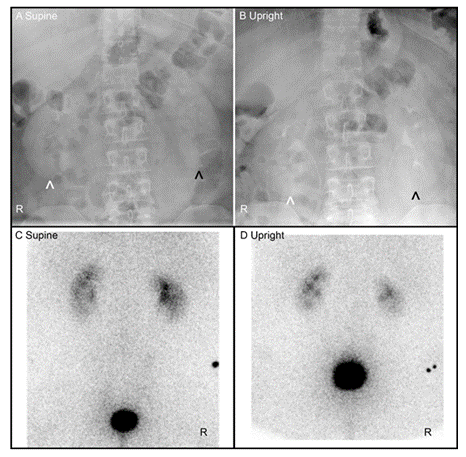
Figure 2: Intravenous pyelogram (IVP) and renal scintigraphy of case 2. Initial supine radiographs after intravenous contrast excretion demonstrated the bilateral kidneys at the expected physiological position (A), the inferior border of the right kidney (white ^ in A) was at the level of L3-L4 intervertebral disk space, the inferior border of the left kidney (black ^ in A) was at the level of L3 inferior endplate. With prolonged standing, there was descent of the right kidney by 2.8 cm with the inferior border of the right kidney (white ^ in B) at the L4 level, and descent of the left kidney by 3.1 cm with the inferior border of the left kidney (black ^ in B) at the L4 level. Renal scintigraphy with Tc-99m DTPA was performed with approximately 180 minutes between the supine position (C) and the upright positon (D), and did not demonstrate supraphysiologic descent of either kidney in the upright position (D).
Table 2: Renal split function of case 2 in the supine and upright positions
|
Right |
Left |
|
|
Supine |
43.20% |
56.80% |
|
Upright |
49.30% |
50.70% |
Case 3
Case 3 was a 44 year-old female who presented with right flank pain and hypertension. IVP showed that in the supine position, the inferior margin of the right kidney was above the superior margin of the right iliac bone (Figure 3A). In the upright position, the right kidney moved inferiorly by approximately 5 cm, the inferior margin of the right kidney was below the superior margin of the right iliac bone (Figure 3B). In the upper pole of the right kidney, there was a single slightly dilated blunted calyx. The reminder of the right and left calyces were unremarkable. Renal scintigraphy with Tc-99m DTPA was performed with approximately 85 minutes between the supine and upright positions. In the supine position, renal scintigraphy showed that the inferior margin of the right kidney was above the superior margin of the right iliac crest (Figure 3C). In the upright position, the right kidney descended, the inferior margin of the right kidney was below the right iliac crest, consistent with right nephroptosis (Figure 3D). The left kidney was relatively larger in size with relatively more blood flow compared to the right kidney. In the supine position, the estimated total GFR was 151 ml/min, the split renal function was 47.0% on the right and 53.0 % on the left. In the upright position, the estimated total GFR was 198 ml/min, the split renal function was 40.4% on the right and 59.6% on the left, suggestive of interval decreased split right renal function (Table 3). The patient underwent robotic assisted laparoscopic right nephropexy and her right flank pain improved.
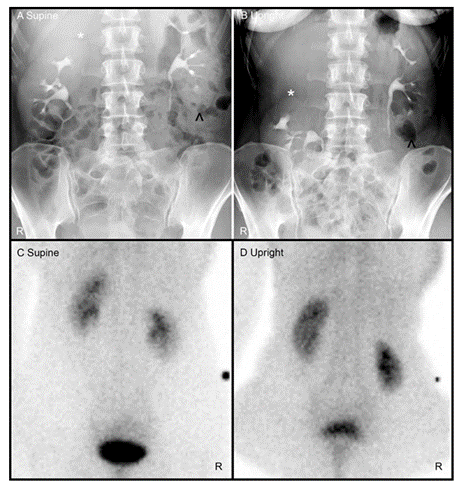
Figure 3: Intravenous pyelogram (IVP) and renal scintigraphy of case 3. IVP showed that in the supine position (A), the superior border of the right kidney (white * in A) was at L2 level, the inferior margin of the right kidney was above the superior margin of the right iliac bone (A). The inferior margin of the left kidney (black ^ in A) was at L4 level in the supine position. In the upright position (B), the right kidney moved inferiorly by approximately 5 cm, the superior border of the right kidney (white * in B) was at L4 level, the inferior margin of the right kidney was below the superior margin of the right iliac bone (B). The inferior margin of the left kidney (black ^ in B) was at L5 level in the upright position. In the upper pole of the right kidney, there was a single slightly dilated blunted calyx. The reminder of the right and left calyces were unremarkable. Renal scintigraphy showed that in the supine position, the inferior margin of the right kidney was above the superior margin of the right iliac crest (C). In the upright position, the right kidney descended, the inferior margin of the right kidney was below the right iliac crest, consistent with right nephroptosis (D).
Table 3: Renal split function of case 3 in the supine and upright positions.
|
Right |
Left |
|
|
Supine |
47.00% |
53.00% |
|
Upright |
40.40% |
59.60% |
Case 4
The fourth patient was a 43 year-old male presented with intermittent gross hematuria, dysuria and bilateral flank pain starting in 2010. He was diagnosed with nephroptosis at an outside institution and underwent staged bilateral nephropexy surgery in 2015 and 2016, with temporary resolution of symptoms for 2 years. His symptoms of gross hematuria, flank pain, voiding dysfunction, sweats, chills and nausea recurred in 2018. Renal scintigraphy in 11/2022 demonstrated recurrent bilateral nephroptosis. Renal scintigraphy with Tc-99m DTPA was performed with approximately 80 minutes between the supine and upright positions. In the supine position, renal scintigraphy showed that the lower pole of both kidneys were above the right iliac crest (Figure 4A). In the upright position, both kidneys descended, the inferior border of the left kidney was at the level of the right iliac crest, the inferior border of the right kidney was below the level of the right iliac crest (Figure 4B). There was normal bilateral renal blood flow and normal bilateral renal function. In the supine position, the estimated total GFR was 127 ml/min, the split renal function was 49.6 % on the right and 50.4 % on the left. In the upright position, the estimated total GFR was 188 ml/min, the split renal function was 43.7 % on the right and 56.3% on the left (Table 4). The patient subsequently underwent robotic bilateral nephropexy in 12/2022, the bilateral renal capsules were tacked to the psoas fascia. Following the repeat nephropexy, the patient’s hematuria symptom resolved and flank pain was improved.
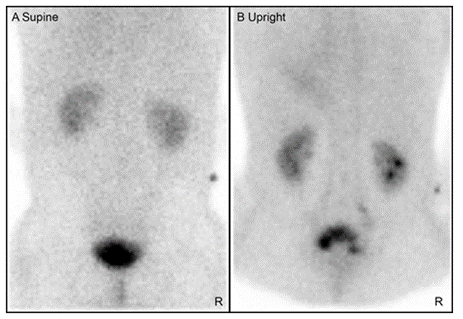
Figure 4: Renal scintigraphy of case 4. In the supine position, renal scintigraphy showed that the lower pole of both kidneys were above the right iliac crest (A). In the upright position, both kidneys descended, the inferior border of the left kidney was at the level of the right iliac crest, the inferior border of the right kidney was below the level of the right iliac crest (B).
Table 4: Renal split function of case 4 in the supine and upright positions
|
Right |
Left |
|
|
Supine |
49.60% |
50.40% |
|
Upright |
43.70% |
56.30% |
Case 5
Case 5 was a 46 year-old female with a history of bilateral flank pain and intermittent gross hematuria. IVP showed that in the supine position at 4 minutes post intravenous contrast injection, the inferior margin of the right kidney was 10.6 cm above the superior margin of the right iliac bone (Figure 5A), and the inferior margin of the left kidney was 9.8 cm above the superior margin of the left iliac bone (Figure 5B). In the upright position at 20 minutes post intravenous contrast injection, the inferior margin of the right kidney was 10.5 cm above the superior margin of the right iliac bone (Figure 5B), and the inferior margin of the left kidney was 8.9 cm above the superior margin of the left iliac bone (Figure 5B). Since the bilateral kidney descended less than 5 cm in the upright position, the IVP radiographic findings were not consistent with nephroptosis. Renal scintigraphy with Tc-99m DTPA was performed with approximately 90 minutes between the supine and upright positions. In the supine position, renal scintigraphy demonstrated that the inferior margin of the bilateral kidneys was above the superior margin of the bilateral iliac crests (Figure 5C). In the upright position, the right kidney descended with its inferior margin below the right iliac crest, consistent with right nephroptosis (Figure 5C). The left kidney also descended at the upright position (Figure 5D). In the supine position, bilateral renal function was normal, the estimated total GFR was 100ml/min, the split renal function was 49.4% on the right and 50.7 % on the left. In the upright position, the estimated total GFR was 107 ml/min, the split renal function was 47.8% on the right and 52.2% on the left, no significant interval change of the renal function compared to the supine position (Table 5). Based upon the nuclear renal scintigraphic evidence of bilateral nephroptosis, the patient underwent robotic assisted bilateral nephropexy, and flank pain was completely gone and the hematuria decreased postsurgery.
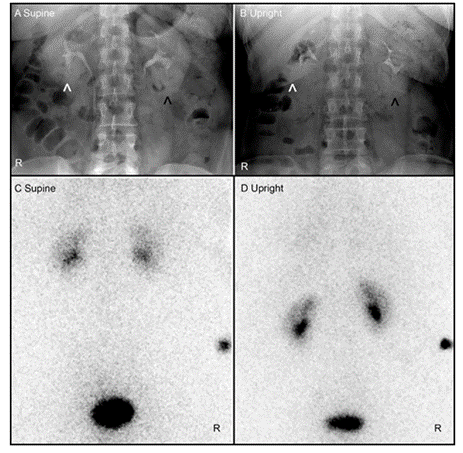
Figure 5: Intravenous pyelogram (IVP) and renal scintigraphy of case 5. IVP showed that in the supine position, the inferior margin of the right kidney (white ^ in A) was 10.6 cm above the superior margin of the right iliac bone (A), and the inferior margin of the left kidney (black ^ in A) was 9.8 cm above the superior margin of the left iliac bone (A). In the upright position, the inferior margin of the right kidney (white ^ in B) was 10.5 cm above the superior margin of the right iliac bone (B), and the inferior margin of the left kidney (black ^ in B) was 8.9 cm above the superior margin of the left iliac bone (B). Since the bilateral kidney descended less than 5 cm in the upright position, the IVP radiographic findings were not consistent with nephroptosis. Renal scintigraphy demonstrated that in the supine position, the inferior margin of the bilateral kidneys was above the superior margin of the bilateral iliac crests (C). In the upright position, the right nephroptosis (D). The left kidney also descended at the upright position (D).
Table 5: Renal split function of case 5 in the supine and upright positions
|
Right |
Left |
|
|
Supine |
49.40% |
50.70% |
|
Upright |
47.80% |
52.20% |
4. Discussion
Nephroptosis is a condition in which a kidney descends greater than two vertebral bodies (or >5 cm) during a position change from supine to upright. In the current study, we evaluated nephroptosis utilizing IVP in combination with nuclear renal scintigraphy. Three cases were consistent with the diagnosis of nephroptosis on IVP, and four cases were consistent with the diagnosis of nephroptosis on renal scintigraphy. One case was not consistent with nephroptosis on either IVP or renal scintigraphy.
Currently, the gold standard diagnostic exam for nephroptosis is visual descent seen on IVP with intravenous contrast after postural change from the supine to the upright position. IVP utilizes X-ray and provides the anatomical location of the kidney based upon the different density of the renal tissue in comparison to the bowel, ribs, and vertebral bodies. Intravenous iodinated contrast further increases the contrast between the kidneys and the adjacent tissues, thereby delineating the border of the kidney and the urinary collecting system. IVP provides high resolution images, and facilitates the quantitative measurement of the distance between the border of the kidney and the iliac bone in both supine and upright positions, as well as evaluates the renal anatomical relationship relative to the vertebral bodies and can show changes in renal axis and orientation. Additionally, renal calyces, renal pelvis, the ureters, and urinary bladder are well visualized in IVP. It allows for the evaluation of other pathology such as calyceal abnormalities, renal papillary necrosis, nephrolithiasis, and hydronephrosis. Boylu and colleagues utilized diuretic renography and reported a case of nephroptosis which exacerbated the degree of ureteropelvic junction obstruction, ultimately requiring robotic pyeloplasty with concomitant nephropexy [13]. The first case in our study showed that the right kidney descended approximately 10 cm into the right pelvis with extensive tortuosity and kinking of the right proximal and mid ureter. These IVP findings alone would identify this patient as a good candidate for surgical correction.
Nuclear renal scintigraphy can evaluate renal size, location, blood flow, renal function as well as urinary obstruction. Several radiotracers have been used for renal scintigraphy. Tc-99m DTPA is cleared via glomerular filtration with no tubular secretion or reabsorption, can be used to estimate glomerular filtration rate (GFR). Tc-99m MAG3 is cleared entirely by tubular secretion, can be utilized to measure effective renal plasma flow (ERPR). Both radiotracer are used to evaluate renal location, blood flow, split renal function, as well as urinary obstruction. To assess the kidney location, our study put a Co-57 source marker at an anterior iliac crest to help evaluate the descent of kidney from the supine position to the upright position. The results of renal scintigraphy are concordant with IVP in the detection of nephroptosis. However, due to the resolution limitation of nuclear renal scintigraphy, it cannot replace IVP the gold standard diagnostic exam of nephroptosis. In our small series, one case was consistent with the diagnosis of nephroptosis on the nuclear renal scintigraphy, but not detected by IVP. For this case, the time interval between the supine position and the upright position on IVP was within 20 minutes, whereas the nuclear renal scintigraphy with Tc-99m DTPA was performed approximated 90 minutes between the supine and upright positions. It should be realized that nephroptosis is a time dependent process. IVP may miss the diagnosis of nephroptosis given the short interval between the supine position and the upright position. The nuclear renal scintigraphy could be performed with a longer time interval between the supine and upright positions, allowing the nephroptotic kidney enough time to descend, and possibly increasing the sensitivity for the diagnosis of nephroptosis.
In addition to anatomic information, nuclear renal scintigraphy is useful to evaluate blood flow and renal function. Dynamic renography imaging is composed of an initial dynamic perfusion imaging sequence, followed by a functional sequence to assess renal uptake and clearance. The differential or split function is the percentage that each kidney contributes to overall function, which is determined at the peak cortical activity. This information can be combined with GFR to evaluate renal function, and help guide clinical management of nephroptosis. Previously, Murari used Tc-99m DTPA renogram reported a case of an inferiorly displaced and malrotated right kidney at the erect position, which was associated with a reduction in the GFR of the affected right kidney [9]. This patient benefited from nephropexy [9]. Similar case was also reported by Carola [14]. Andriole and colleagues reported reduction of GFR in the erect position in 10 of 13 patients with either unilateral or bilateral nephroptosis, suggesting that GFR measurement can be helpful in evaluating nephroptosis [15]. Similarly, our first patient with symptom of right flank pain was diagnosed with right nephroptosis on IVP, renal scintigraphy reconfirmed right nephroptosis and demonstrated interval decreased split renal function and decreased estimated GFR of the right ptotic kidney in the upright position. Although this may be related to postural change of renal function, the change in the depth and anterior-posterior rotation of the ptotic kidney in the upright position may affect the measurement of split renal function and GFR measurement by Gates’ method. Gates’ method is a gamma camera-based method with Tc-99m DTPA to measure GFR. This method may be affected by the geographic change of the kidney, specifically, the renal depth is the most important factor that influences the GFR calculated by Gates’ method [11, 16]. The third patient in the current study had right kidney nephroptosis on both IVP and renal scintigraphy, with interval decreased split right renal function with the postural change from the supine to the upright position, ultimately underwent robotic right nephropexy. The decreased calculated split right renal function may be related to postural change of renal function.
In addition to Tc-99m DTPA renal scintigraphy, nuclear renal scan with Tc-99m MAG3 and Tc-99m glucoheptonate (Tc-99m GHA) are also able to detect nephroptosis and evaluate renal function and drainage. Kumar and colleagues utilizing Tc-99m GHA renal scintigraphy detected a case of right-sided nephroptosis when the patient was standing during preoperative evaluation as a living kidney donor [17]. Temizkan and colleagues utilizing Tc-99m MAG3 renogram demonstrated 4 cases of nephroptosis who presented with renovascular hypertension but no evidence of stenosis of the renal arteries on the digital subtraction angiography, the renogram demonstrated diminished perfusion and excretion on the affected nephroptotic side, thereafter all 4 patients received nephropexy and became normotensive [18]. This case report suggested that renal scintigraphy may be a preferred diagnostic method for cases of renovascular hypertension due to nephroptosis [18].
Furthermore, diuretic renal scintigraphy can facilitate the diagnosis of nephroptosis. Tartaglione and colleagues assessed 36 patients with unilateral or bilateral hydronephrosis, utilized Tc-99m MAG3 diuretic renography with two diuretic protocols [19]. In the supine position, diuretic was injected intravenously 15 min before (F-15) radionuclide administration [19]. Later in a seated position, the patient drunk 400 to 500 mL of water at 5 minutes and received an injection of 20 mg of furosemide at 10 minutes after [F+10 (sp)] radionuclide administration [19]. In the seated position, they observed nephroptosis in 22.2% of kidneys in 36 patients by F+10 (sp) [19]. Diuretic renal scintrigraphy is therefore applicable for the diagnosis of nephroptosis. Theoretically, diuretic renal scintigraphy is useful in the evaluation of complications associated with nephroptosis such as secondary ureteropelvic junction obstruction, which will need further validation.
5. Conclusion
Nuclear renal scintigraphy offers an accessible, valuable, and novel means to better evaluate nephroptosis in the preoperative setting. In addition to the anatomic information provided via IVP, renal scintigraphy can provide supplementary information regarding renal blood flow and function, which may aid urologists in the selection of potential nephropexy candidates, perioperative management as well as surgical planning. This protocol may require further optimization and standardization of time interval between scans at the supine positon and the upright positon. A Co-57 marker can be utilized to locate the anterior iliac crest to help evaluate the change of the renal anatomical location. The nuclear renal scintigraphy could be performed with longer interval between the supine and upright positions, to allow the nephroptotic kidney enough time to migrate inferiorly and better capture the degree of descent, and possibly improve the sensitivity for the detection of nephroptosis. Further study is in need to validate this protocol prior to implementation into routine clinical practice and extension to diuretic renal scintigraphy.
Conflicting Interests:
Dr. Daniel D Eun: 1) Intuitive surgical: consultant, speaker, teaching activities. 2) Hitachi Medical/Fuji Film: grant support. 3) Melzi Corp: Shareholder. All other authors declare no conflicts of interest.
References
- Yoshida S, Matsumura M, Maekawa K, et al. Recurrent abdominal pain caused by nephroptosis. Clin J Gastroenterol 13 (2020): 621-625.
- Ghanem AN. Features and complications of nephroptosis causing the loin pain and hematuria syndrome. A preliminary report. Saudi Med J 23 (2002): 197-205.
- de Zeeuw D, Donker AJ, Burema J, et al. Nephroptosis and hypertension. Lancet 1 (1977): 213-215.
- Buffardi A, Ceruti C, Destefanis P, et al. Nefropessi retroperitoneoscopica [Retroperitoneoscopic nephropexy]. Urologia 77 (2010): 16-20.
- Vodopija N, Korsic L, Zupancic M, et al. Is laparoscopic nephropexy improving the quality of life. Coll Antropol 31 (2007): 689-692.
- Chan VSH, Lam TPW, Lam WWM. Nephroptosis: The wandering kidney. Kidney Res Clin Pract 37 (2018): 306-307.
- Barber NJ, Thompson PM. Nephroptosis and nephropexy--hung up on the past? Eur Urol 46 (2004): 428-433.
- Strohmeyer DM, Peschel R, Effert P, et al. Changes of renal blood flow in nephroptosis: assessment by color Doppler imaging, isotope renography and correlation with clinical outcome after laparoscopic nephropexy. Eur Urol 45 (2004): 790-793.
- Murari SB, Gadepalli T, Rao VP, et al. Renal scintigraphy in diagnosis and management of nephroptosis. Indian J Nucl Med 27 (2012): 52-54.
- Wang K, Fan M, Shao F, et al. Nephroptosis Incidentally Found on 99m Tc-DTPA Renal Dynamic Scan. Clin Nucl Med 47 (2022): 1099-1100.
- Gates GF. Glomerular filtration rate: Estimation from fractional renal accumulation of 99mTc-DTPA (stannous). AJR Am J Roentgenol 138 (1982): 565-570.
- Blaufox MD, De Palma D, Taylor A, et al. The SNMMI and EANM practice guideline for renal scintigraphy in adults. Eur J Nucl Med Mol Imaging 45 (2018): 2218-2228.
- Boylu U, Lee BR, Thomas R. Robotic-assisted laparoscopic pyeloplasty and nephropexy for ureteropelvic junction obstruction and nephroptosis. J Laparoendosc Adv Surg Tech A 19 (2009): 379-382.
- Carola F. Renal ptosis and change of glomerular filtration values in the upright and supine positions. Clin Nucl Med 28 (2003): 150-153.
- Andriole VT, Bonadio M, Bianchi C. The influence of postural changes on the glomerular filtration rate in nephroptosis. Yale J Biol Med 47 (1974): 268-276.
- Awdeh M, Kouris K, Hassan IM, et al. Factors affecting the Gates' measurement of glomerular filtration rate. Am J Physiol Imaging 5 (1990): 36-41.
- Kumar R, Gupta R, Reddy SN, et al. Nephroptosis: the Tc-99m glucoheptonate scan as a diagnostic method. Clin Nucl Med 25 (2000): 473.
- Temizkan M, Wijmenga LF, Ypma AF, et al. Nephroptosis: a considerable cause of renovascular hypertension. Neth J Med 47 (1995): 61-65.
- Tartaglione G, D'Addessi A, De Waure C, et al. (99m)Tc-MAG3 diuretic renography in diagnosis of obstructive nephropathy in adults: a comparison between F-15 and a new procedure F+10(sp) in seated position. Clin Nucl Med 38 (2013): 432-436.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 75.63%
Acceptance Rate: 75.63%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
