Unexpected Elevation of Infection Parameters in a Heart Transplanted Patient with Chronic Kidney Disease: A Case Report
Kurzhagen JT¹, Roeder SS¹, Müller-Deile J¹*
1Department of Nephrology and Hypertension, Friedrich-Alexander University Erlangen-Nuremberg, Erlangen, Germany
*Corresponding Author: Janina Müller-Deile, Department of Nephrology and Hypertension, Friedrich-Alexander University Erlangen-Nuremberg, Erlangen, Germany.
Received: 31 October 2022; Accepted: 18 November 2022; Published: 30 November 2022
Article Information
Citation: Kurzhagen JT, Roeder SS, Müller-Deile J. Unexpected Elevation of Infection Parameters in a Heart Transplanted Patient with Chronic Kidney Disease: A Case Report. Archives of Clinical and Medical Case Reports 6 (2022): 763-765.
View / Download Pdf Share at FacebookAbstract
Patients with end-stage kidney disease are under an increased risk for morbidity and mortality due to cardiovascular reasons. Yet, patients might show only atypical symptoms during cardiac events and routinely performed pre-transplant diagnostic measures are discussed controversially. A heart transplanted 50-year-old male with end-stage kidney disease was assessed for kidney transplantation. Myocardial scintigraphy, chest x-ray, pulmonary function test, urological and gastrointestinal assessment showed normal results. A routinely performed blood test revealed elevated procalcitonin, C-reactive protein and leucocytes. Measured vital parameters and physical examination revealed no pathologies. Coughing, shortness of breath or chest pain were denied. CT-scan showed no signs of infection but lack of contrast media enhancement in the heart. Myocardial infarction was confirmed in electrocardiogram and transthoracic echocardiogram demonstrated an impaired ejection fraction of 20%. Treatment with anti-platelet medication and anticoagulation was followed by invasive heart catheterization, which revealed no acute stenosis but a dissolved in-stent thrombosis. Since kidney failure was progressing the patient required dialysis treatment. Microbiological analyses of blood and urine samples stayed negative. Chronic kidney disease patients are at increased cardiovascular risk. However, invasiveness of cardiac diagnostics for potential kidney transplant is debated controversially. KDIGO guideline 2020 advises non-invasive screening for coronary artery disease for asymptomatic patients at high risk. However, there is no specific guideline for previously heart transplanted candidates for kidney transplant and patients with high pretest probability benefit from invasive diagnostics. A risk stratification for cardiac complications and pre-kidney transplant evaluation should be executed in clinical practice.
Keywords
Complication; Coronary Artery Disease; Heart Transplant; Kidney Transplant; Invasive Screening; Non-Invasive Screening
Complication articles; Coronary Artery Disease articles; Heart Transplant articles; Kidney Transplant articles; Invasive Screening articles; Non-Invasive Screening articles
Complication articles Complication Research articles Complication review articles Complication PubMed articles Complication PubMed Central articles Complication 2023 articles Complication 2024 articles Complication Scopus articles Complication impact factor journals Complication Scopus journals Complication PubMed journals Complication medical journals Complication free journals Complication best journals Complication top journals Complication free medical journals Complication famous journals Complication Google Scholar indexed journals COVID-19 articles COVID-19 Research articles COVID-19 review articles COVID-19 PubMed articles COVID-19 PubMed Central articles COVID-19 2023 articles COVID-19 2024 articles COVID-19 Scopus articles COVID-19 impact factor journals COVID-19 Scopus journals COVID-19 PubMed journals COVID-19 medical journals COVID-19 free journals COVID-19 best journals COVID-19 top journals COVID-19 free medical journals COVID-19 famous journals COVID-19 Google Scholar indexed journals Coronary Artery Disease articles Coronary Artery Disease Research articles Coronary Artery Disease review articles Coronary Artery Disease PubMed articles Coronary Artery Disease PubMed Central articles Coronary Artery Disease 2023 articles Coronary Artery Disease 2024 articles Coronary Artery Disease Scopus articles Coronary Artery Disease impact factor journals Coronary Artery Disease Scopus journals Coronary Artery Disease PubMed journals Coronary Artery Disease medical journals Coronary Artery Disease free journals Coronary Artery Disease best journals Coronary Artery Disease top journals Coronary Artery Disease free medical journals Coronary Artery Disease famous journals Coronary Artery Disease Google Scholar indexed journals Ultrasound articles Ultrasound Research articles Ultrasound review articles Ultrasound PubMed articles Ultrasound PubMed Central articles Ultrasound 2023 articles Ultrasound 2024 articles Ultrasound Scopus articles Ultrasound impact factor journals Ultrasound Scopus journals Ultrasound PubMed journals Ultrasound medical journals Ultrasound free journals Ultrasound best journals Ultrasound top journals Ultrasound free medical journals Ultrasound famous journals Ultrasound Google Scholar indexed journals Heart Transplant articles Heart Transplant Research articles Heart Transplant review articles Heart Transplant PubMed articles Heart Transplant PubMed Central articles Heart Transplant 2023 articles Heart Transplant 2024 articles Heart Transplant Scopus articles Heart Transplant impact factor journals Heart Transplant Scopus journals Heart Transplant PubMed journals Heart Transplant medical journals Heart Transplant free journals Heart Transplant best journals Heart Transplant top journals Heart Transplant free medical journals Heart Transplant famous journals Heart Transplant Google Scholar indexed journals Kidney Transplant articles Kidney Transplant Research articles Kidney Transplant review articles Kidney Transplant PubMed articles Kidney Transplant PubMed Central articles Kidney Transplant 2023 articles Kidney Transplant 2024 articles Kidney Transplant Scopus articles Kidney Transplant impact factor journals Kidney Transplant Scopus journals Kidney Transplant PubMed journals Kidney Transplant medical journals Kidney Transplant free journals Kidney Transplant best journals Kidney Transplant top journals Kidney Transplant free medical journals Kidney Transplant famous journals Kidney Transplant Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals SRAS-CoV-2 articles SRAS-CoV-2 Research articles SRAS-CoV-2 review articles SRAS-CoV-2 PubMed articles SRAS-CoV-2 PubMed Central articles SRAS-CoV-2 2023 articles SRAS-CoV-2 2024 articles SRAS-CoV-2 Scopus articles SRAS-CoV-2 impact factor journals SRAS-CoV-2 Scopus journals SRAS-CoV-2 PubMed journals SRAS-CoV-2 medical journals SRAS-CoV-2 free journals SRAS-CoV-2 best journals SRAS-CoV-2 top journals SRAS-CoV-2 free medical journals SRAS-CoV-2 famous journals SRAS-CoV-2 Google Scholar indexed journals Invasive Screening articles Invasive Screening Research articles Invasive Screening review articles Invasive Screening PubMed articles Invasive Screening PubMed Central articles Invasive Screening 2023 articles Invasive Screening 2024 articles Invasive Screening Scopus articles Invasive Screening impact factor journals Invasive Screening Scopus journals Invasive Screening PubMed journals Invasive Screening medical journals Invasive Screening free journals Invasive Screening best journals Invasive Screening top journals Invasive Screening free medical journals Invasive Screening famous journals Invasive Screening Google Scholar indexed journals Treatment articles Treatment Research articles Treatment review articles Treatment PubMed articles Treatment PubMed Central articles Treatment 2023 articles Treatment 2024 articles Treatment Scopus articles Treatment impact factor journals Treatment Scopus journals Treatment PubMed journals Treatment medical journals Treatment free journals Treatment best journals Treatment top journals Treatment free medical journals Treatment famous journals Treatment Google Scholar indexed journals
Article Details
Abbreviations:
CAD- Coronary Artery Disease; CKD- Chronic Kidney Disease; CRP- C-Reactive Protein; CT- Computed Tomography; ECG- Electrocardiogram; EF- Ejection Fraction; ESRD- End-Stage Kidney Disease; KT- Kidney Transplant; PCT- Procalcitonin; STEMI- ST-Elevation Myocardial Infarction
1. Introduction
The immense increase in mortality of patients with end-stage kidney disease (ESRD) is mainly due to cardiovascular reasons [1]. Before potential kidney transplantation, non-invasive diagnostic workup is not validated and the current KDIGO guideline is discussed controversially [1]. In this paper, we describe the case of a previously heart transplanted male with chronic kidney disease (CKD) presenting a major complication during the pre-kidney transplant assessment phase. This rare case points out the need for individual cardiac diagnostic workup prior to KT based on specific risk and pretest probability. Additionally, we outline atypical symptoms, laboratory parameters and discuss the relevance of contrast-induced nephropathy.
2. Case Presentation
A 50-year-old heart transplanted male with CKD stage G4A3 was admitted for kidney transplant (KT) evaluation. Orthotropic heart transplantation had been performed 9 years earlier due to transposition of the great arteries. The etiologies of CKD were calcineurin inhibitor toxicity, cardio-renal syndrome and secondary focal segmental glomerular sclerosis. The patient was stable throughout the hospital stay and routine examinations were performed for evaluation as KT candidate, such as myocardial scintigraphy, chest x-ray, lung function test, urology, and gastrointestinal assessment which were all unremarkable. However, on the day of planned hospital discharge, elevated infection parameters including C-reactive protein (CRP), procalcitonin (PCT) as well as transaminases, creatine kinase and lactate dehydrogenase were detected (day 0, Table 1).
|
Parameter |
2022/01/31 |
2022/02/04 |
2022/02/05 |
|
Leucocytes 103/ μl |
5.5 |
10.2 |
18.9 |
|
CRP mg/l |
15 |
108.7 |
272 |
|
PCT ng/ml |
- |
1 |
17.3 |
Table 1: Laboratory parameters.
Table 1 displays leucocyte counts (in 103 cells/µl), PCT (in ng/ml) and CRP (in mg/l) levels for day -4, day 0 and day 1.
Interestingly, the patient had no fever, showed stable cardiovascular and respiratory conditions, clinical examination was unremarkable and urine assessment showed no sign for infection. The patient denied symptoms such as pain, coughing, shortness of breath and alguria. Urine and blood cultures were collected and sent out to microbiology. Aerococcus urinae was detected in the patient’s urine while blood culture tests remained negative. Antibiotic treatment with intravenous piperacillin/tazobactam was initiated. Since infectious parameters were further increasing on the next day (day 1, table 1), a thoracic and abdominal contrast-enhanced CT-scan was performed to find the focus of infection. The CT- scan showed myocardial infarction in the left anterior descending artery territory, a new apical aneurysm and a left ventricular thrombus (Figure 1). Repeated electrocardiogram (ECG) recordings showed newly elevated ST segments (Figure 2).
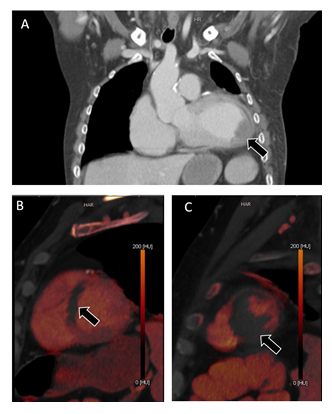
Figure 1: CT-scan. Representative images of the contrast-enhanced thoracic CT-scan. A Coronal image of the left ventricle revealing apical aneurysm and left ventricular thrombus (arrow). B and C Sagittal images of CT-based iodine imaging. The arrows depict hypoperfusion of the septal and apical myocardium.
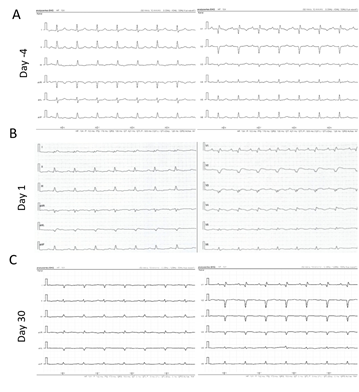
Figure 2: ECG. Three consecutive ECG recordings. A Routine ECG recording from 4 days prior to the event. B ECG recording performed immediately after the CT-scan revealing myocardial infarction. ST-segment elevation is present in leads I, II, aVL, V1-V5 (day 1). C Follow-up ECG recording 30 days after the event.
Maximum Troponin levels were >125.000 pg/ml and creatine kinase >140 U/l. The ejection fraction (EF) decreased from >55% 4 days before to 25% in transthoracic echocardiogram. Treatment with aspirin and heparin was initiated immediately. Heart catheter was postponed because of the fear that contrast media would lead to CKD progression to ESRD and because myocardial infarction most likely ran its course somedays before. However, even without further contrast media the patient required hemodialysis treatment due to acute on chronic kidney injury because of impaired cardiac output. When heart catheter was finally performed, no stenosis but a potential former in-stent thrombosis was detected. A control echocardiography showed a slightly improved but still dramatically impaired EF of 30-35%. Upon hospital discharge, the patient still required dialysis treatment. Blood and urine cultures remained sterile.
3. Discussion and Conclusions
This case report has several teaching aspects: First, CKD is a major cardiovascular risk factor [1]. Therefore, prior to listing for KT patients with CKD often receive cardiac diagnostic workup which, however, is not validated for detection of coronary artery disease (CAD) in this population. Studies comparing invasive vs. non-invasive cardiac diagnostics prior to KT delivered controversial results and current pretransplant screening guidelines are only based on expert opinions [1]. Guidelines recommend non-invasive CAD screening for asymptomatic patients prior to listing for KT [2]. A meta-analysis found invasive coronary angiography and non-invasive measures to be comparable when detecting major adverse cardiac events. However, sensitivity and specificity were low for non-invasive diagnostics and a substantial number of people with negative test results went on to experience adverse cardiac events [3]. Therefore, in asymptomatic patients before and after KT, non-invasive diagnostics are not suitable to rule out CAD as all these tests do not have a sufficient likelihood ratio and no sufficient posttest probability can be achieved. Asymptomatic patients with high pretest probability should directly undergo angiography. For symptomatic patients coronary angiography is the first choice as well [4]. Regarding therapeutic approaches, coronary revascularization is not superior to optimal medical therapy in reducing mortality or major adverse cardiovascular events in waitlisted KT candidates with CAD [5].
Thus, more detailed algorithms based on risk stratification and therapy should be elaborated [6]. Second, CKD patients as well as heart transplanted patients may present with atypical symptoms when suffering from myocardial ischemia [7]. This calls for an increased awareness for more atypical signs such as abnormal laboratory findings. Third, elevation of infection parameters including PCT can be a sign of myocardial infarction in the absence of infection. PCT has been identified as an earlier marker than CK-MB and Troponin I, however, not necessarily correlating with the amount of myocardial tissue injury [8]. In patients with severe ST-elevation myocardial infarction (STEMI) and cardiogenic shock, PCT values are significantly increased [9]. Myocardial infarction leads to a sterile inflammation and reduced perfusion of the bowels can induce transient leakage of the intestinal barrier with transient bacteremia stimulating PCT and other infection parameters [8]. Fourth, whether contrast media causes AKI was lately called into question, even though CKD has been identified as major risk factor. However, the risk of contrast-associated AKI has been overestimated in the past and there is a risk of underusing otherwise necessary interventions such as percutaneous coronary intervention. Potential lifesaving diagnostics and intervention should not be delayed because of a risk of AKI [10].
Acknowledgement
N/A
Conflicts of Interest
The authors have declared that no conflict of interest exists.
References
- Hart A, Weir MR, Kasiske BL. Cardiovascular risk assessment in kidney transplantation. Kidney Int 87 (2015): 527-534.
- Chadban SJ, Ahn C, Axelrod DA, et al. KDIGO Clinical Practice Guideline on the Evaluation and Management of Candidates for Kidney Transplantation. Transplantation 104 (2020): S11-S103.
- Wang LW, Masson P, Turner RM, et al. Prognostic value of cardiac tests in potential kidney transplant recipients: a systematic review. Transplantation 99 (2015): 731-745.
- Pauker SG, Kassirer JP. The threshold approach to clinical decision making. N Engl J Med 302 (1980): 1109-1117.
- Siddiqui MU, Junarta J, Marhefka GD. Coronary Revascularization Versus Optimal Medical Therapy in Renal Transplant Candidates With Coronary Artery Disease: A Systematic Review and Meta-Analysis. J Am Heart Assoc 11 (2022): e023548.
- Kassab K, Doukky R. Cardiac imaging for the assessment of patients being evaluated for kidney transplantation. J Nucl Cardiol 29 (2022): 543-557.
- Gao SZ, Schroeder JS, Hunt SA, et al. Acute myocardial infarction in cardiac transplant recipients. Am J Cardiol 64 (1989): 1093-1097.
- Reindl M, Tiller C, Holzknecht M, et al. Association of Myocardial Injury With Serum Procalcitonin Levels in Patients With ST-Elevation Myocardial Infarction. JAMA Netw Open 3 (2020): e207030.
- Picariello C, Lazzeri C, Chiostri M, et al. Procalcitonin in patients with acute coronary syndromes and cardiogenic shock submitted to percutaneous coronary intervention. Intern Emerg Med 4 (2009): 403-408.
- Mehran R, Dangas GD, Weisbord SD. Contrast-Associated Acute Kidney Injury. N Engl J Med 380 (2019): 2146-2155.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 75.63%
Acceptance Rate: 75.63%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
