Pediatric Acute Respiratory Distress Syndrome and Sepsis in Children with Dravet Syndrome Following Upper Respiratory Tract Infections
Friederike Schwarz1*, Gabriela Oesch2, Christoph Aebi3, Elisabeth Kieninger4, Thomas Riedel1
1Department of Paediatrics, Division of Paediatric Intensive Care Medicine, Inselspital, Bern University Hospital, University of Bern, Switzerland
2Department of Paediatrics, Division of Neuropaediatrics, Development and Rehabilitation, Inselspital, Bern University Hospital, University of Bern, Switzerland
3Department of Paediatrics, Division of Paediatric Infectious Diseases, Inselspital, Bern University Hospital, University of Bern, Switzerland
4Department of Paediatrics, Division of Paediatric Respiratory Medicine and Allergology, Inselspital, Bern University Hospital, University of Bern, Switzerland
*Corresponding Author: Friederike Schwarz, Department of Paediatrics, Division of Paediatric Intensive Care Medicine, Inselspital, Bern University Hospital, University of Bern, Switzerland
Received: 12 January 2024; Accepted: 22 January 2024; Published: 13 February 2024
Article Information
Citation: Friederike Schwarz, Gabriela Oesch, Christoph Aebi, Elisabeth Kieninger, Thomas Riedel. Pediatric Acute Respiratory Distress Syndrome and Sepsis in Children with Dravet Syndrome Following Upper Respiratory Tract Infections. Archives of Clinical and Medical Case Reports. 8 (2024): 23-25.
View / Download Pdf Share at FacebookAbstract
Herein we report on four children with SCN1A related Dravet syndrome (DS) with severe pediatric acute respiratory distress syndrome (PARDS) and sepsis following upper respiratory infections that have occurred in clusters over a short period of time. Complications included PARDS with need of veno-venous extracorporeal membrane oxygenation (VV-ECMO) and acute kidney injury treated with continuous veno-venous hemodiafiltration (CVVHDF). This striking observations warrant further exploration of DS patients’ susceptibility to respiratory tract infections.
Keywords
Dravet syndrome; SCN1A mutation; Respiratory infections; PARDS; Sepsis; Multi-organ failure
Dravet syndrome articles; SCN1A mutation articles; Respiratory infections articles; PARDS articles; Sepsis articles; Multi-organ failure articles.
Dravet syndrome articles Dravet syndrome Research articles Dravet syndrome review articles Dravet syndrome PubMed articles Dravet syndrome PubMed Central articles Dravet syndrome 2023 articles Dravet syndrome 2024 articles Dravet syndrome Scopus articles Dravet syndrome impact factor journals Dravet syndrome Scopus journals Dravet syndrome PubMed journals Dravet syndrome medical journals Dravet syndrome free journals Dravet syndrome best journals Dravet syndrome top journals Dravet syndrome free medical journals Dravet syndrome famous journals Dravet syndrome Google Scholar indexed journals Syndrome articles Syndrome Research articles Syndrome review articles Syndrome PubMed articles Syndrome PubMed Central articles Syndrome 2023 articles Syndrome 2024 articles Syndrome Scopus articles Syndrome impact factor journals Syndrome Scopus journals Syndrome PubMed journals Syndrome medical journals Syndrome free journals Syndrome best journals Syndrome top journals Syndrome free medical journals Syndrome famous journals Syndrome Google Scholar indexed journals SCN1A mutation articles SCN1A mutation Research articles SCN1A mutation review articles SCN1A mutation PubMed articles SCN1A mutation PubMed Central articles SCN1A mutation 2023 articles SCN1A mutation 2024 articles SCN1A mutation Scopus articles SCN1A mutation impact factor journals SCN1A mutation Scopus journals SCN1A mutation PubMed journals SCN1A mutation medical journals SCN1A mutation free journals SCN1A mutation best journals SCN1A mutation top journals SCN1A mutation free medical journals SCN1A mutation famous journals SCN1A mutation Google Scholar indexed journals Respiratory infections articles Respiratory infections Research articles Respiratory infections review articles Respiratory infections PubMed articles Respiratory infections PubMed Central articles Respiratory infections 2023 articles Respiratory infections 2024 articles Respiratory infections Scopus articles Respiratory infections impact factor journals Respiratory infections Scopus journals Respiratory infections PubMed journals Respiratory infections medical journals Respiratory infections free journals Respiratory infections best journals Respiratory infections top journals Respiratory infections free medical journals Respiratory infections famous journals Respiratory infections Google Scholar indexed journals PARDS articles PARDS Research articles PARDS review articles PARDS PubMed articles PARDS PubMed Central articles PARDS 2023 articles PARDS 2024 articles PARDS Scopus articles PARDS impact factor journals PARDS Scopus journals PARDS PubMed journals PARDS medical journals PARDS free journals PARDS best journals PARDS top journals PARDS free medical journals PARDS famous journals PARDS Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals Sepsis articles Sepsis Research articles Sepsis review articles Sepsis PubMed articles Sepsis PubMed Central articles Sepsis 2023 articles Sepsis 2024 articles Sepsis Scopus articles Sepsis impact factor journals Sepsis Scopus journals Sepsis PubMed journals Sepsis medical journals Sepsis free journals Sepsis best journals Sepsis top journals Sepsis free medical journals Sepsis famous journals Sepsis Google Scholar indexed journals Multi-organ failure articles Multi-organ failure Research articles Multi-organ failure review articles Multi-organ failure PubMed articles Multi-organ failure PubMed Central articles Multi-organ failure 2023 articles Multi-organ failure 2024 articles Multi-organ failure Scopus articles Multi-organ failure impact factor journals Multi-organ failure Scopus journals Multi-organ failure PubMed journals Multi-organ failure medical journals Multi-organ failure free journals Multi-organ failure best journals Multi-organ failure top journals Multi-organ failure free medical journals Multi-organ failure famous journals Multi-organ failure Google Scholar indexed journals
Article Details
1. Introduction
Severe complications of pulmonary infections in patients with DS have been reported previously [1 - 4], however, might be still underestimated in the pediatric patients [3]. Only a few studies reported on the role of specific pathogens [1, 2], however, the exact pathophysiologic mechanisms of the severe reaction to simple upper respiratory infections in DS patients still need to be clarified [1, 4]. The impact of respiratory infections on morbidity and outcome in children with DS due to SCN1A mutation will be highlighted in the following case series.
2. Case Series
Four patients aged 5.5 years (median, range 1.5 - 13.7) with SCN1A related Dravet syndrome were admitted to the PICU of the Bern University Hospital between February and May 2023: three of them presented with rapid respiratory deterioration due to pediatric acute respiratory distress syndrome (PARDS) and one with sepsis secondary to pleuropneumonia (table 1). Pathogens identified included Influenza type B and enterovirus. All of the children had upper respiratory tract infections in the weeks prior to admission. Two of the ARDS patients required one VV-ECMO run for 5 and 11 days, respectively (Figure 1). Oxygenation index was > 25 in all ARDS patients (median 67, range 29 – 68) and mechanical ventilation was needed for 14 days (median, range 5 – 16). All patients were under inotropic support for median 4 days (range 3 – 6). One of the ECMO patients was treated with CVVHDF for acute kidney injury for 10 days. Renal function normalized after ECMO weaning. Short seizures were witnessed in two patients, EEG ruled out status epilepticus. Neuroimaging (cerebral MRI or CT) was performed in three patients excluding bleeding and ischemia. The already before admission installed antiepileptic combination therapy was continued. Antibiotic agents were given for 13 days (median, range 6 – 16 days), blood cultures remained negative in all patients. Thrombocytopenia was present in all patients, two patients were pancytopenic. Length of stay at PICU was 15 days (median, range 6 – 26 days), length of hospital stay 24 days (median, range 11 – 35). None of the patients died. Recovery from the acute illness was heterogenic and required weeks to months. At time of discharge all patients showed increased muscular weakness and fatigue compared to their baseline before hospitalization; one of the ECMO patients suffered from critical illness myopathy.
Table 1: Patients’ characteristics
|
Patient |
1 |
2 |
3 |
4 |
|
Age |
1 y 8 mo |
1 y 6 mo |
9 y 6 mo |
13 y 8 mo |
|
Sex |
m |
m |
m |
f |
|
Antiepileptic medication |
valporic acid, stiripentol, clobazam |
valporic acid, stiripentol, clobazam |
valporic acid, clobazam, topiramate |
valporic acid, stiripentol, clobazam, topiramate |
|
Main diagnosis of hospital stay |
Sepsis |
PARDS |
PARDS |
PARDS |
|
Duration of illness before ICU admission (d) |
8 |
5 |
6 |
4 |
|
Length of stay, PICU (d) |
6 |
21 |
9 |
26 |
|
Length of stay, hospital (d) |
20 |
28 |
11 |
35 |
|
Mechanical ventilation (d) |
- |
16 |
5 |
14 |
|
VV-ECMO (d) |
- |
11 |
- |
5 |
|
CVVHDF (d) |
- |
10 |
- |
- |
|
Inotrops (d) |
4 |
3 |
3 |
6 |
|
Length of antibiotic treatment (d) |
10 |
16 |
6 |
16 |
|
Transfusion of RBC / TC |
- / + |
+ / + |
- / - |
+ / + |
|
pSOFA score at PICU admission |
12 |
14 |
16 |
14 |
|
Oxygenation index at PICU admission |
- |
68 |
29 |
67 |
|
CRP (max., g/l) |
121 |
240 |
43 |
390 |
|
Pathogenes identified: acute (weeks before admission) |
Enterovirus |
- (Picornavirus, parainfluenza virus) |
Influenza type B |
Candida albicans (EBV) |
ARDS = acute respiratory distress syndrome; CVVHDF = continuous veno-venous hemodiafiltration; d = days; EBV = Epstein Barr virus; f = female; m = male; mo = months; PICU = pediatric intensive care unit; pSOFA score = pediatric sequential organ failure assessment score; RBC = red blood cells; TC = thrombocytes; VV-ECMO = veno-venous extracorporeal membrane oxygenation; y = years
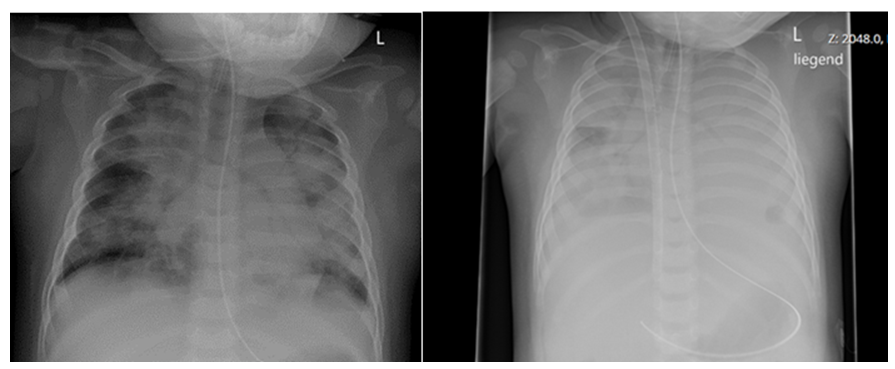
Figure 1: Chest X-ray at admission to PICU with signs of severe PARDS (left side) and X-ray after jugular VV-ECMO cannulation via dual-lumen cannula (right side) of the same patient following rapid respiratory deterioration few hours later.
3. Discussion
Few studies report the impact of respiratory tract infections in patients with DS [1, 2]. Howell et al demonstrated the neurologic complications and sequelae caused by Influenza infections in 24 patients [1]. Clinical findings were similar to those in our patients, including pneumonia, ARDS and acute kidney injury. They reported one death (4.2%), caused by pneumonia. Bjurulf et al found a mortality rate of respiratory infections as high as 5.7% (3/53 children) in pediatric DS patients [3]. The survey of Balestrini et al regarding the impact of COVID-19 infection on the DS population in the UK showed a good outcome and low infection rate due to early prevention measures [2]. Takastuki et al reported a case of a girl with deletion 2q24.2 including the SCN1A mutation with severe pulmonary emphysema secondary to pneumonia [4]. They suspected the pulmonary complication to be caused by the loss of the integrin β6 gene (ITGB6).
Until now there is no clear understanding of the underlying pathophysiology in DS with respiratory infections and severe clinical course leading to PARDS. In our case series we demonstrate four cases of severe multi-organ dysfunction following respiratory infections in children with SCN1A related Dravet syndrome. Patients suffered life-threatening complications including respiratory and kidney failure as well as long-term neurologic sequelae. We were surprised by the rapid progression and the severity of the patients’ course (figure 1). Pathogens were identified in two of the patients, differed from patient to patient (Influenza type B, enterovirus) and were not age-dependent. It is likely that DS patients’ pulmonary vulnerability is not limited to a special pathogen or age-group but might be more likely related to its underlying genetic constellation. The gene SCN1A is primarily expressed in the brain and also in the lungs, thus might play a crucial role in pathogenesis of severe pulmonary disease [5].
4. Conclusion
The striking observations of PARDS and sepsis in Dravet patients warrants further exploration of DS patients’ susceptibility to respiratory tract infections. Due to the potential of rapid clinical deterioration we strongly recommend treating DS patients with caution when identifying respiratory infection, such as early antibiotic treatment and PICU consultation.
Acknowledgements and Funding
Not applicable.
Conflicts of Interests
The authors of this article have no conflicts of interest.
References
- Howell KB, Butcher S, Schneider AL, Russ-Hall S, Muzariri PR, et al. Complications of Influenza A or B Virus Infection in Individuals With SCN1A-Positive Dravet Syndrome. Neurology 100 (2023): e435-e442.
- Balestrini S, Wilson G, Eldred C, Evans H, Sisodiya SM. The impact of COVID-19 in Dravet syndrome: A UK survey. Acta Neurol Scand 143 (2021): 389-395.
- Bjurulf B, Reilly C, Sigurdsson GV, Thunström S, Kolbjer S, et al. Dravet syndrome in children-A population-based study. Epilepsy Res 182 (2022): 106922.
- Takatsuki S, Nakamura R, Haga Y, Mitsui K, Hashimoto T, et al. Severe pulmonary emphysema in a girl with interstitial deletion of 2q24.2q24.3 including ITGB6. Am J Med Genet Part A 152 (2010): 1020–1025.
- The Human Protein Atlas (2023).


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 75.63%
Acceptance Rate: 75.63%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
