Mobile Cloud-Based 12-Lead ECG Transmission during Helicopter Transport of STElevation Myocardial Infarction Patients
Makoto Onodera1*, Tomotaka Misawa2, Kotaro Sorimachi2, Ken Iseki2, Takeshi Shimizu3, Takayoshi Yamaki3, Yasuchika Takeishi3, Keiji Sakamoto4, Hiroki Hosaka5, Hiroyuki Mizukami6, Masahiro Ono7
1Department of regional emergency medicine, Fukushima Medical University, 1 Hikarigaoka, Fukushima City, Fukushima, 960-1295 Japan
2Department of emergency medicine, school of medicine, Fukushima Medical University, 1 Hikarigaoka, Fukushima City, Fukushima, 960-1295 Japan
3Department of cardiovascular medicine, school of medicine, Fukushima medical university, 1 Hikarigaoka, Fukushima City, Fukushima, 960-1295 Japan
4Division of cardiology, Hoshi General Hospital, 159-1 Mukaigawaramachi, Koriyama City, Fukushima, 963-8501 Japan
5Division of cardiology, Aidu Chuo Hospital, 1-1 Tsuruga-machi, Aizuwakamatsu City, Fukushima, 965-8611 Japan
6Division of cardiology, Jusendo General Hospital, 1-1-17 Ekimae, Koriyama City, Fukushima, 963-8585 Japan
7Department of cardiology, Southern of Tohoku General Hospital, 7-115 Yatsuyamada, Koriyama City, Fukushima, 963-8563 Japan
*Corresponding Author: Makoto Onodera, Department of regional emergency medicine, Fukushima Medical University, 1 Hikarigaoka, Fukushima City, Fukushima, 960-1295 Japan
Received: 22 September 2025; Accepted: 02 October 2025; Published: 23 October 2025
Article Information
Citation: Makoto Onodera, Tomotaka Misawa, Kotaro Sorimachi, Ken Iseki, Takeshi Shimizu, Takayoshi Yamaki, Yasuchika Takeishi, Keiji Sakamoto, Hiroki Hosaka, Hiroyuki Mizukami, Masahiro Ono. Mobile Cloud-Based 12-Lead ECG Transmission during Helicopter Transport of STElevation Myocardial Infarction Patients. Archives of Clinical and Medical Case Reports. 9 (2025): 210-216.
View / Download Pdf Share at FacebookAbstract
Delayed reperfusion therapy for ST-segment elevation myocardial infarction (STEMI) is associated with high mortality rates. Although mobile cloud-based 12-lead electrocardiogram (MC-ECG) systems have shown promise in reducing treatment delays, their implementation remains limited in regions where geographic and institutional constraints hinder timely interventions. This study aimed to evaluate the effectiveness of helicopter emergency medical services (HEMS) equipped with an MCECG system in reducing the time to reperfusion and improving shortterm outcomes in patients with STEMI. This retrospective observational study included patients with STEMI transported via HEMS in Fukushima Prefecture between July 2022 and August 2024. The inclusion criterion was confirmation of ST elevation by a flight physician using MC-ECG at rendezvous points (RPs) with subsequent percutaneous coronary intervention (PCI) at a receiving facility. The measured outcomes included the time from symptom onset to emergency medical service contact, contact with the flight physician, transport times, door-to-balloon time (DTBT), and 30-day survival. Among the 1,087 HEMS dispatches, 15 STEMI cases met the inclusion criteria. The median patient age was 59 years, and 80% of the patients were men. The median DTBT was 57 min and the 30-day survival rate was 100%. Air transport was significantly faster than predicted ground transport (median 12 vs. 61 min, p < 0.01). The integration of MC-ECG into the HEMS enabled the rapid diagnosis and transport of patients with STEMI to PCI-capable facilities, achieving DTBT within guideline-recommended timeframes and excellent short-term outcomes. This approach may be particularly beneficial in geographically dispersed regions with limited cardiological resources.
Keywords
<p>Pre-hospital 12-lead electrocardiogram; Flight physician; Rendezvous point; Door-to-balloon time</p>
Article Details
1. Introduction
In patients with ST-segment elevation myocardial infarction (STEMI), delayed reperfusion therapy is associated with increased mortality [1]. The Japanese Circulation Society and American Heart Association guidelines emphasize that the door-to-balloon time (DTBT), defined as the interval from arrival at a medical facility to the initiation of reperfusion, should occur within 90 min [2, 3]. A recently developed mobile cloud-based 12-lead electrocardiogram (MC-ECG) system has enabled the transmission of ECG data from ambulances via bluetooth and mobile networks [4, 5]. Cardiologists can thus remotely access ECGs in real time, thereby enabling the prompt mobilization of emergency catheterization teams. This system reduces the relative risk of 30-day mortality in patients with STEMI [6, 7]. However, according to the Ministry of Health, Labour and Welfare, the Fukushima Prefecture exhibited the highest age-adjusted mortality rate for acute myocardial infarction (AMI) in both men and women in 2017, remaining above the national average [8]. A 2021 report on 973 patients with AMI in Fukushima indicated an average time from symptom onset to hospital arrival of 444 min and a mean DTBT of 280 min [9]. Despite these delays, only a few emergency medical services (EMS) in the prefecture have implemented MC-ECG systems.
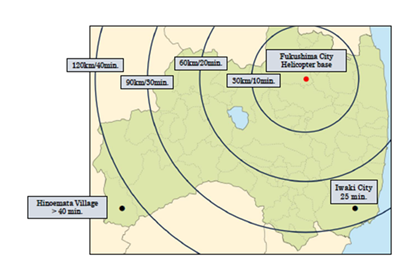
Fukushima Medical University has operated a helicopter emergency medical service (HEMS) since January 2008. The air ambulance’s maximum flight time has been over 40 minutes for Hinoemata Village and over 25 minutes for Iwaki City, to provide emergency coverage across the entire prefecture (Figure 1).
From its inception to December 2024, the HEMS completed 6,260 missions, including 388 trips in 2024. In July 2022, an MC-ECG system was installed in an air ambulance, to enable flight physicians to perform ECGs at rendezvous points (RPs) and coordinate with percutaneous coronary intervention (PCI)-capable hospitals before transportation. In this study, we investigated individuals with STEMI for whom ST elevation was confirmed by a flight physician using MC-ECG, the data were transmitted to a receiving hospital, and the patients were transported via HEMS. We focused on the time to reperfusion and clinical outcomes across five PCI-capable facilities with access to a cloud ECG system.
2. Materials and Methods
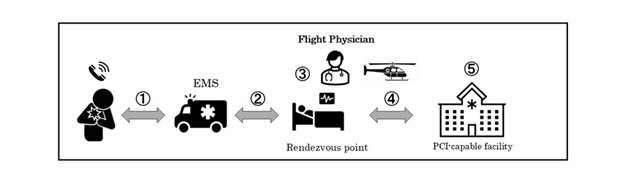
We retrospectively analyzed patients with STEMI from July 2022 to August 2024 in which a flight physician confirmed ST-segment elevation using MC-ECG at RPs, and the patient subsequently underwent PCI. The following study items were measured: time from symptom onset to EMS contact, time from EMS contact to flight physician contact, time from flight physician contact to RP take-off (on-site activity time), flight transport time, estimated ground transport time using Google Maps (Google Inc., Mountain View, CA, USA), total time from symptom onset to hospital arrival, high-sensitivity troponin I (hs-TnI) levels, DTBT, and 30-day survival rate (Figure 2).
1) Time from symptom onset to EMS contact (min.)
2) Time from EMS contact to flight physician contact (min.)
3) Time from flight physician contact to RPs take-off (on-site activity time) (min.)
4) Flight transport time (min.)
Comparison with estimated ground transport time (min.)
5) High-sensitivity troponin I level (pg/mL), door-to-balloon time (min.), and 30-day survival rate
EMS, emergency medical services; RPs, rendezvous points; PCI, percutaneous coronary intervention
The HEMS used was an Eurocopter EC135, a twin-engine general-purpose helicopter manufactured by Eurocopter (now Airbus Helicopters). The MC-ECG (SCUNA) is a cloud-based prehospital data-sharing system developed by the MEHERGEN Group (Fukuoka, Japan). At the RPs, the flight physician performed a 12-lead ECG, transmitted the data to the receiving facility, and confirmed the availability of PCI. Based on the Japanese guidelines for acute coronary syndrome (ACS) (2), nitrates or antiplatelet agents were administered as indicated. The receiving hospitals included Hospital A in Fukushima City (helicopter base); Hospitals B, C, and D in Koriyama City; and Hospital E in Aizu-Wakamatsu City, all equipped to receive MC-ECG transmissions in advance (Figure 3).
Statistical analyses were performed using Statcel (3rd edition; OMS Publishing). Data are presented as medians and interquartile ranges (IQR). The Wilcoxon signed-rank test was used to compare flight and estimated ground transport times. Spearman’s rank correlation was used to assess the relationship between time to hospital arrival and hs-TnI levels. Statistical significance was set at p < 0.05.
3. Results
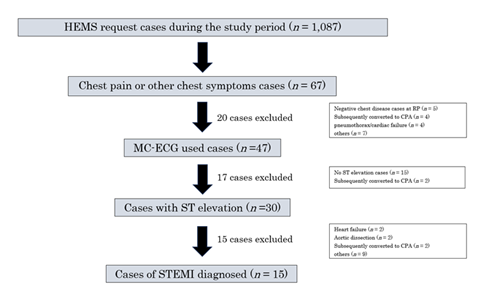
During the study period, the HEMS was dispatched 1,087 times and transported 67 patients with chest symptoms. MC-ECG was used in 47 patients, after excluding 20 patients with negative chest disease at the time of contact with a flight physician. ST-segment elevation was confirmed in 30 patients, excluding 15 patients without ST-segment elevation and two who later experienced cardiopulmonary arrest. Ultimately, 15 patients were diagnosed with STEMI and underwent PCI (Figure 4).
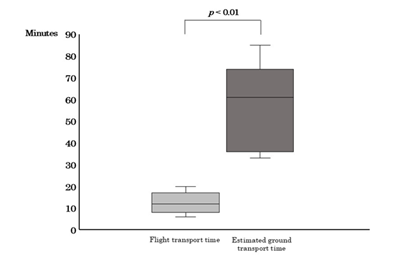
Among the study cohort, 12 patients were men and three were women, with a median age of 59 years (IQR: 54–72 years). The median time from symptom onset to EMS contact was 109 (42–191) minutes and the median time from EMS contact to flight physician contact was 30 (20–34) minutes. In contrast, the on-site activity time was 16 (12–22) min, during which 12-lead ECGs were performed and transmitted, and transfer to a PCI-capable hospital was confirmed before take-off. Five patients received nitrate or antiplatelet agents at RPs. The median flight transport time was 12 min (range, 8–17 min) and the estimated ground transport time was 61 min (range, 36–74 min). The median DTBT was 57 min (range, 43–77 min) and the 30-day survival rate was 100% (Table 1).
Table 1: Baseline characteristics of patients in this study
EMS, emergency medical service; RPs, rendezvous points; IQR, interquartile range; APA, antiplatelet agent
Additionally, the flight transport time was significantly shorter than the estimated ground transport time (p <0.01; Figure 5).
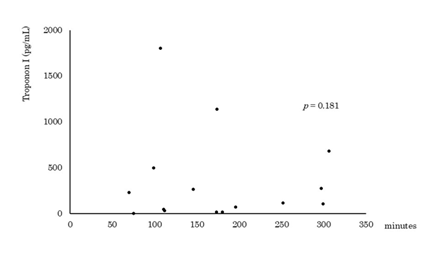
Furthermore, no significant correlation was found between total time to hospital arrival and hs-TnI levels (p = 0.181; Figure 6).
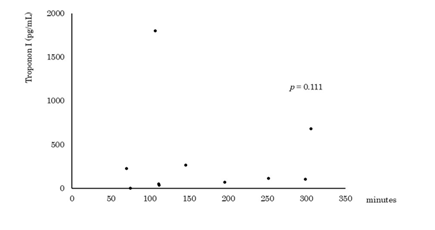
A sub-analysis of 10 patients who were not treated with nitrates or antiplatelet agents also showed no significant correlation with arrival time and outcomes (p = 0.111; Figure 7).
4. Discussion
All patients with STEMI in this study achieved a DTBT within 90 min and had favorable outcomes. Several studies have reported on the use of HEMS for transport of patients with AMI [10-12]. Youngquist et al. [10] reported that 85% of patients with STEMI were transferred to PCI-capable facilities within 2 h based on 35 HEMS records across the United States. Regarding the effectiveness of MC-ECG, Hata et al. [11] reported a reduced time from hospital arrival to intervention due to pre-arrival information provided by flight staff, whereas Diercks et al. [12] reported not only a reduction in DTBT but also an improvement in the outcomes. Funder et al. [13] reported a 30-day mortality rate of 5.0% in 384 patients with suspected STEMI who were transported via HEMS. In their study, the median DTBT was 31 min; however, the flight transport time to a PCI-capable medical institution was 71 min. In our study, the median flight transport time was only 12 min, and all patients achieved a DTBT of <90 min, suggesting a favorable prognosis. This efficiency was likely due to the advance coordination of flight physician with PCI-capable institution.
Additionally, the flight transport time was significantly shorter than the predicted ground transport time. Studies have consistently shown that HEMS significantly reduces transport times compared to ground EMS. For example, one analysis found a significant reduction in transport time for 384 HEMS cases compared to 1,220 ground cases (p =0.004) [13], while others reported similar significant improvements in smaller cohorts (p < 0.001 and p < 0.05) [14, 15]. Given Fukushima’s limited PCI-capable facilities and long ground transport times, the advantages of pre-arrival communication via MC-ECG and flight transport are particularly relevant.
No correlation was found between the total time from symptom onset to hospital arrival and hs-TnI levels. TnI essential for the diagnosing and assessing the risk of AMI, with hs-TnI particularly useful for improving diagnostic accuracy in the early stages [16-18]. Keller et al. [16] reported that hs-TnI measured with 3 h of symptom onset had a sensitivity of 88% and a specificity of 96% in 1,818 patients with chest pain. In this study, 12 of the 15 patients showed elevated hs-TnI levels, although values varied widely, and no significant correlation emerged between the total time from symptom onset and hospital arrival. Furthermore, no correlation was found among 10 patients who were not treated with nitrates or antiplatelet agents at the RPs. The Japanese guidelines for ACS prioritize immediate reperfusion based on clinical and ECG findings rather than waiting for biomarker confirmation [2, 19]. Therefore, prompt transport of patients with ST-segment elevation to PCI-capable facilities remains essential.
In this study, the time from symptom onset to EMS contact was 109 min. Erol et al. [20] reviewed 643 AMI cases in Turkey and found that only 272 (43.8%) patients were admitted within 12 h of symptom onset, attributing to delay to public low awareness of EMS benefits and myocardial infarction symptoms. Similarly, Meischke et al. [21] reported low EMS utilization due to patients lack of awareness of life-threatening symptoms. In Fukushima Prefecture, a 2021 analysis of AMI cases reported a mean delay of 444 min from symptom awareness to hospital arrival [9]. In the present study, this interval was shortened to 173 min; however, the median time from symptom onset to EMS contact remained 109 min, underscoring the need to reduce pre-EMS delay. These findings highlight the importance of public education on AMI symptoms and the urgency of early EMS activation.
This study has several limitations. First, this was a single-institution retrospective study. Second, the number of cases was small and various biases could not be excluded. Third, treatment varies among flight physicians, with no uniform activity. Finally, patients were not always transported to the nearest PCI-capable facility.
5. Conclusion
In regions with limited MC-ECG implementation, an HEMS equipped with cloud-based ECG transmission can facilitate rapid diagnosis, prompt PCI coordination, and timely reperfusion, contributing to favorable short-term outcomes in patients with STEMI.
Ethics approval and consent to participate
This study adhered to the Declaration of Helsinki and was approved by the Ethics Committee of the School of Medicine at Fukushima Medical University (approval number: 2024-108). The requirement for written informed consent was waived as the obtained data was de-identified.
Acknowledgments
We would like to thank Dr. Keiichiro Maeda, Dr. Shinichi Konno, and Dr. Jun Sakuma who contributed to this study as the directors of the collaborating medical institutions.
Conflicts of interest
The authors have no external support information or financial interests relevant to this content to disclose.
References
- Arinaga T, Suematsu Y, Nakamura A, et al. The Effectiveness of Mobile Cloud 12-Lead Electrocardiogram Transmission System in Patients with ST-Segment Elevation Myocardial Infarction. Medicina (Kaunas) 58 (2022): 247.
- Kimura K, Kimura T, Ishihara M, et al. JCS 2018 Guideline on Diagnosis and Treatment of Acute Coronary Syndrome. Circ J 83 (2019): 1085–1196.
- O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 127 (2013): e362–e425.
- Fujita H, Uchimura Y, Waki K, et al. Development and Clinical Study of Mobile 12-Lead Electrocardiography Based on Cloud Computing for Cardiac Emergency. Stud Health Technol Inform 192 (2013): 1077.
- Takeuchi I, Fujita H, Yanagisawa T, et al. Impact of Doctor Car with Mobile Cloud ECG in reducing door-to-balloon time of Japanese ST-elevation myocardial infarction patients. Int Heart J 56 (2015): 170-173.
- Welsford M, Nikolaou NI, Beygui F, et al. Part 5: Acute Coronary Syndromes: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Circulation 132: (2015) S146-S176.
- Van’t Hof AW, Rasoul S, van de Wetering H, et al. Feasibility and benefit of prehospital diagnosis, triage, and therapy by paramedics only in patients who are candidates for primary angioplasty for acute myocardial infarction. Am Heart J 151 (2006): 1255.e1-5.
- Fukushima Prefecture Homepage (2025).
https://www.pref.fukushima.lg.jp/sec/21045c/kyuuseisinnkinnkousoku-jittai.html.
- Fukushima Prefecture Homepage (2025).
http://www.pref.fukushima.lg.jp/sec/21045a/hukushimakennbannkennkoude-tabe-su.html#jyunkanki
- Youngquist ST, McIntosh SE, Swanson ER, et al. Air ambulance transport times and advanced cardiac life support interventions during the interfacility transfer of patients with acute ST-segment elevation myocardial infarction. Prehosp Emerg Care 14 (2010): 292-299.
- Hata N, Kobayashi N, Imaizumi T, et al. Use of an air ambulance system improves time to treatment of patients with acute myocardial infarction. Intern Med 45 (2006): 45-50.
- Diercks DB, Kontos MC, Chen AY, et al. Utilization and impact of pre-hospital electrocardiograms for patients with acute ST-segment elevation myocardial infarction: data from the NCDR (National Cardiovascular Data Registry) ACTION (Acute Coronary Treatment and Intervention Outcomes Network) Registry. J Am Coll Cardiol 53 (2009): 161-166.
- Funder KS, Rasmussen LS, Siersma V, et al. Helicopter vs. ground transportation of patients bound for primary percutaneous coronary intervention. Acta Anaesthesiol Scand 62 (2018): 568-578.
- Jang JY, Kwon WK, Roh H, et al. Time-saving effects using helicopter transportation: comparison to a ground transportation time predicted using a social navigation software. Medicine (Baltimore) 100 (2021): e26569.
- Stassen W, Tsegai A, Kurland L. A Retrospective Geospatial Simulation Study of Helicopter Emergency Medical Services' Potential Time Benefit Over Ground Ambulance Transport in Northern South Africa. Air Med J 42 (2023): 440-444.
- Keller T, Zeller T, Peetz D, et al. Sensitive troponin I assay in early diagnosis of acute myocardial infarction. N Engl J Med 361 (2009): 868-877.
- Lee KK, Doudesis D, Ferry AV, et al. High-STEACS Investigators. Implementation of a high sensitivity cardiac troponin I assay and risk of myocardial infarction or death at five years: observational analysis of a stepped wedge, cluster randomised controlled trial. BMJ 383 (2023): e075009.
- Neumann JT, Twerenbold R, Ojeda F, et al. COMPASS-MI Study Group. Application of High-Sensitivity Troponin in Suspected Myocardial Infarction. N Engl J Med 380 (2019): 2529-2540.
- Luepker RV, Apple FS, Christenson RH, et al. Case definitions for acute coronary heart disease in epidemiology and clinical research studies: a statement from the AHA Council on Epidemiology and Prevention; AHA Statistics Committee; World Heart Federation Council on Epidemiology and Prevention; the European Society of Cardiology Working Group on Epidemiology and Prevention; Centers for Disease Control and Prevention; and the National Heart, Lung, and Blood Institute. Circulation 108 (2003): 2543–2549.
- Erol MK, Kayıkçıoğlu M, Kılıçkap M, et al. Time delays in each step from symptom onset to treatment in acute myocardial infarction: Results from a nation-wide TURKMI registry. Anatol J Cardiol 25 (2021): 294-303.
- Meischke H, Ho MT, Eisenberg MS, et al. Reasons patients with chest pain delay or do not call 911. Ann Emerg Med 25 (1995): 193–197.



 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 75.63%
Acceptance Rate: 75.63%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
