Arthroscopic Fixation of ACL and PCL Avulsion with Medial Tibial Plateau Fracture in a Patient with Osteogenesis Imperfecta
Tessanya Gunatilake1*, Joel Smith2
1University of California, Berkeley, California, USA
2 Department of Orthopaedic, Musculoskeletal and Joint Research Foundation, San Diego, California, USA
*Corresponding Author: Tessanya Gunatilake, University of California, Berkeley, California, USA
Received: 30 August 2025; Accepted: 08 September 2025; Published: 06 October 2025
Article Information
Citation: Tessanya Gunatilake, Joel Smith. Arthroscopic Fixation of ACL and PCL Avulsion with Medial Tibial Plateau Fracture in a Patient with Osteogenesis Imperfecta. Archives of Clinical and Medical Case Reports. 9 (2025): 187-189.
View / Download Pdf Share at FacebookAbstract
Osteogenesis imperfecta is a rare genetic connective tissue disorder resulting in bone fragility. We present a unique case of an avulsion of both the anterior cruciate and posterior cruciate ligaments, along with a medial tibial plateau fracture in a patient with osteogenesis imperfecta and vascular complications. Our case highlights the challenges of managing traumatic knee injuries complicated by bone fragility and vascular risks, underscoring the importance of a multidisciplinary approach for effective fixation.
Keywords
<p>Osteogenesis imperfecta; Anterior cruciate ligament avulsion; Posterior cruciate ligament avulsion; Tibial plateau fracture; Arthroscopic internal fixation</p>
Article Details
1. Background
Osteogenesis imperfecta (OI) is a genetic connective tissue disorder characterized by impaired synthesis of type I collagen, resulting in decreased bone strength and increased susceptibility to fractures [1,2]. Knee injuries involving avulsion of the anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), and a medial tibial plateau fracture are uncommon and typically result from high-energy trauma [3,4]. Management becomes further complicated in patients with OI, where bone fragility limits fixation options [5]. We present a unique case of arthroscopic internal fixation in a patient with OI who sustained a multiligamentous knee injury and tibial plateau fracture [6, 7].
2. Case Presentation
A 44-year-old male with a known history of osteogenesis imperfecta sustained a traumatic injury to his left knee in a motorcycle accident. He reported increasing pain and swelling in the left leg, along with a cold sensation in his left foot compared to the right. On physical examination, the patient was alert and hemodynamically stable. Inspection revealed tenderness in the proximal left knee.
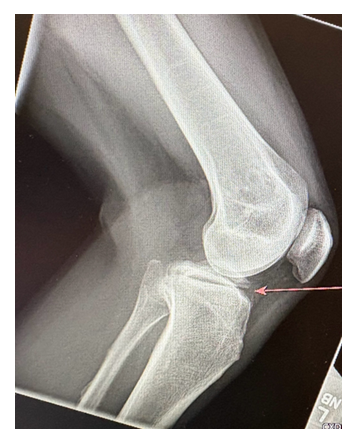
Radiography of the knee revealed a transverse fracture through the proximal tibial metaphysis, with minimal soft tissue swelling and no joint effusion. A non-contrast CT was obtained for further evaluation, which confirmed fractures of both the distal femur and proximal tibia, along with a moderately-sized hemarthrosis. A mildly displaced avulsion fracture was identified at the anterolateral tibia.
Magnetic resonance imaging revealed a tibial eminence fracture fragment measuring 4.2 cm x 4.4 cm, involving the attachment sites of both the anterior and posterior cruciate ligaments.
Additionally, there was evidence of a complete rupture of the medial collateral ligament. Vascular imaging identified an acute deep venous thrombosis (DVT) in the peroneal vein.
Due to the increased risk of thromboembolism, an inferior vena cava (IVC) filter was placed preoperatively. Surgical management was performed the following day under general anesthesia. An anterolateral portal was created, and superolateral outflow was established. A longitudinal incision was made, and soft tissue and hematoma were cleared using cautery and shaver to expose the fracture site. With the knee in flexion, an arthroscopic grasper was used to reduce the fracture fragment. An ACL drill guide was positioned to maintain the reduction. Arthroscopic visualization confirmed successful reduction, and a guide wire was inserted into the ACL footprint. A 4 mm reamer was used to create a tunnel through which a TightRope device was passed to secure the fracture. The implant was engaged, and with application of tension, the fracture remained stable. Fluoroscopic imaging confirmed secure engagement of the button with the ACL fibers and successful flipping of the button. Final reduction was verified under imaging, and the wound was closed with Monocryl and Dermabond.
Postoperative management included knee immobilization and physical therapy for mobilization with an assistive device as needed. DVT prophylaxis was continued under the guidance of the primary care provider.
3. Discussion
This case demonstrates the successful use of arthroscopic internal fixation to manage an ACL and PCL avulsion and a tibial plateau fracture in a patient with OI. The minimally invasive approach enabled effective stabilization while minimizing surgical risk. Preoperative identification of DVT and placement of an IVC filter highlight the importance of multidisciplinary management. This case highlights how specialized surgical strategies can facilitate successful treatment in patients with complex orthopedic injuries and reduced bone integrity.
Disclosure:
The authors report no conflict of interest related to this work
References
- Katsman A, Strauss EJ, Campbell KA, et al. Posterior cruciate ligament avulsion fractures. Curr Rev Musculoskelet Med 11 (2018): 503-509.
- White EA, Patel DB, Matcuk GR, et al. Cruciate ligament avulsion fractures: Anatomy, biomechanics, Injury Patterns, and approach to management. Emerg Radiol 20 (2013): 429-440.
- Sundararajan SR, Rajasekaran S, Bernard SL. Displaced Anterior cruciate ligament avulsion fractures: Arthroscopic staple fixation. Indian Journal of orthopaedics 45 (2011): 324-329.
- US Department of Health and Human Services. Osteogenesis imperfecta. National Institute of Arthritis and Musculoskeletal and Skin Diseases (2025).
- Villaseñor Valdés JJ, Muñoz Nieto D, García Estrada EI, et al. Surgical management of a proximal tibial epiphyseal fracture in a pediatric patient with osteogenesis imperfecta. Cureus 17 (2025): e84131.
- Strevel EL, Papaioannou A, Adachi JD, et al. Case report: Osteogenesis imperfecta elusive cause of fractures. Can Fam Physician 51 (2005): 1655-1657.
- Ren J, Xu X, Jian X, et al. Osteogenesis imperfecta type I: A case report. Exp Ther Med 7 (2014): 1535-1538.




 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 75.63%
Acceptance Rate: 75.63%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
