Atypical Presentation of a Large Aortopulmonary Window in a Very Low Weight and Preterm Born Infant
Katja Schumacher, Sabine Meier, Michael A Borger, Martin Kostelka, Marcel Vollroth
Department of Cardiac Surgery, Heart Center, HELIOS Clinic, University Hospital Leipzig, Leipzig, Germany
*Corresponding Author: Marcel Vollroth, Department of Cardiac Surgery, Heart Center, HELIOS Clinic, University Hospital Leipzig, Leipzig, Germany.
Received: 21 March 2022; Accepted: 05 April 2022; Published: 13 May 2022
Article Information
Citation: Katja Schumacher, Sabine Meier, Michael A Borger, Martin Kostelka, Marcel Vollroth. Atypical Presentation of a Large Aortopulmonary Window in a Very Low Weight and Preterm Born Infant. Archives of Clinical and Medical Case Reports 6 (2022): 370-373.
View / Download Pdf Share at FacebookKeywords
Aortopulmonary; Cardiac malformations; Surgery
Aortopulmonary articles Aortopulmonary Research articles Aortopulmonary review articles Aortopulmonary PubMed articles Aortopulmonary PubMed Central articles Aortopulmonary 2023 articles Aortopulmonary 2024 articles Aortopulmonary Scopus articles Aortopulmonary impact factor journals Aortopulmonary Scopus journals Aortopulmonary PubMed journals Aortopulmonary medical journals Aortopulmonary free journals Aortopulmonary best journals Aortopulmonary top journals Aortopulmonary free medical journals Aortopulmonary famous journals Aortopulmonary Google Scholar indexed journals COVID-19 articles COVID-19 Research articles COVID-19 review articles COVID-19 PubMed articles COVID-19 PubMed Central articles COVID-19 2023 articles COVID-19 2024 articles COVID-19 Scopus articles COVID-19 impact factor journals COVID-19 Scopus journals COVID-19 PubMed journals COVID-19 medical journals COVID-19 free journals COVID-19 best journals COVID-19 top journals COVID-19 free medical journals COVID-19 famous journals COVID-19 Google Scholar indexed journals Cardiac malformations articles Cardiac malformations Research articles Cardiac malformations review articles Cardiac malformations PubMed articles Cardiac malformations PubMed Central articles Cardiac malformations 2023 articles Cardiac malformations 2024 articles Cardiac malformations Scopus articles Cardiac malformations impact factor journals Cardiac malformations Scopus journals Cardiac malformations PubMed journals Cardiac malformations medical journals Cardiac malformations free journals Cardiac malformations best journals Cardiac malformations top journals Cardiac malformations free medical journals Cardiac malformations famous journals Cardiac malformations Google Scholar indexed journals Surgery articles Surgery Research articles Surgery review articles Surgery PubMed articles Surgery PubMed Central articles Surgery 2023 articles Surgery 2024 articles Surgery Scopus articles Surgery impact factor journals Surgery Scopus journals Surgery PubMed journals Surgery medical journals Surgery free journals Surgery best journals Surgery top journals Surgery free medical journals Surgery famous journals Surgery Google Scholar indexed journals Ultra Sound articles Ultra Sound Research articles Ultra Sound review articles Ultra Sound PubMed articles Ultra Sound PubMed Central articles Ultra Sound 2023 articles Ultra Sound 2024 articles Ultra Sound Scopus articles Ultra Sound impact factor journals Ultra Sound Scopus journals Ultra Sound PubMed journals Ultra Sound medical journals Ultra Sound free journals Ultra Sound best journals Ultra Sound top journals Ultra Sound free medical journals Ultra Sound famous journals Ultra Sound Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals SARS articles SARS Research articles SARS review articles SARS PubMed articles SARS PubMed Central articles SARS 2023 articles SARS 2024 articles SARS Scopus articles SARS impact factor journals SARS Scopus journals SARS PubMed journals SARS medical journals SARS free journals SARS best journals SARS top journals SARS free medical journals SARS famous journals SARS Google Scholar indexed journals malformations articles malformations Research articles malformations review articles malformations PubMed articles malformations PubMed Central articles malformations 2023 articles malformations 2024 articles malformations Scopus articles malformations impact factor journals malformations Scopus journals malformations PubMed journals malformations medical journals malformations free journals malformations best journals malformations top journals malformations free medical journals malformations famous journals malformations Google Scholar indexed journals Syndrome Corona articles Syndrome Corona Research articles Syndrome Corona review articles Syndrome Corona PubMed articles Syndrome Corona PubMed Central articles Syndrome Corona 2023 articles Syndrome Corona 2024 articles Syndrome Corona Scopus articles Syndrome Corona impact factor journals Syndrome Corona Scopus journals Syndrome Corona PubMed journals Syndrome Corona medical journals Syndrome Corona free journals Syndrome Corona best journals Syndrome Corona top journals Syndrome Corona free medical journals Syndrome Corona famous journals Syndrome Corona Google Scholar indexed journals
Article Details
1. Introduction
With a prevalence of only 0.2-0.3% of all congenital cardiac malformations, aortopulmonary window is a rare but surgically correctable anomaly [1]. It is caused by the incomplete fusion of two conotruncal ridges that usually separate the embryonal truncus arteriosus into the aorta and pulmonary artery [1]. Frequently, aortopulmonary window is associated with other cardiac anomalies such as arch abnormalities, transposition of the great arteries, ventricular septal defects and tetralogy of Fallot [1-3]. Due to similar hemodynamic, differential diagnosis may include large ductus arteriosus and truncus arteriosus [1]. Because of the left-to-right-shunt, the defect leads to increased pulmonary blood flow following congestive heart failure, pulmonary hypertension and failure to thrive [1]. Depending on the size of the defect, the majority of patients suffer from severe clinical symptoms at young age, for example tachycardia, fatigue, tachypnea and increased respiratory symptoms with recurrent infections [2]. Surgery is indicated as soon as the diagnosis is made to prevent fixed pulmonary hypertension [1].
2. Case presentation
A one-month old premature born and low-weight (1348 g) female infant (born at gestational age 32+1) presented intubated and ventilated with progredient signs of heart failure and recurrent respiratory infections since birth. Clinical examination revealed a systolic murmur at the left sternal border. Echocardiography (Figure 1) and cardiac catherization (Figure 2) showed a large atypical aortopulmonary window >6mm located between the pulmonary artery bifurcation and the ascending aorta extending to the aortic arch.
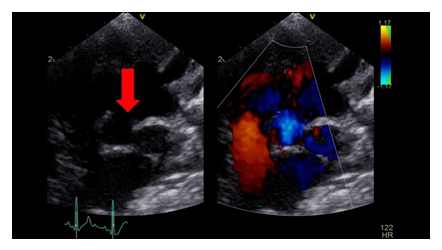
Figure 1: The echocardiographic examination illustrates the very large defect with a significant left to right shunt. The red arrow marks the discontinuity between the aortic arch and the roof of the main pulmonary artery.
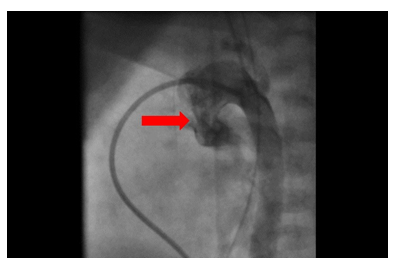
Figure 2: Cardiac catheterization confirmed the very large atypical configurated Aortopulmonary window (red arrow).
The pressure in the right ventricle was nearly systemic, pulmonary artery pressure was very high (80/31-51). Additionally, echocardiography demonstrated an ostium secundum atrial septal defect with significant left to right shunt. Both ventricles were dilated, the right ventricle presented hypertrophic. Based on the clinical symptoms and the diagnostic findings, surgical correction was indicated. Surgery was performed 23 days before the expected delivery date. At the time of surgery, the weight of the infant was 2000g. Access was through median sternotomy; cardiopulmonary bypass was established with aorto-right- atrial cannulation. Surgery was performed in deep hypothermic circulatory arrest (18°C). Neuromonitoring was assessed with cerebral oximeter. The pulmonary arteries were snared, and aortic cross clamp was applied. Cardiac arrest was induced administering antegrade St. Thomas cardioplegia (30ml/kg/BW). The bypass was stopped for 25 minutes. After aortotomy, the location of the aortopulmonary window was identified and closed with autologous pericardial patch in sandwich-patch closure technique. The atrial septal defect was closed by direct suture. Cardiopulmonary bypass was re-started, and the patient was warmed up and weaned off bypass. The postoperative course was prolonged due to respiratory insuffiency with subsequent prolonged mechanical ventilation. There was no evidence of pulmonary hypertension. Chest X-ray demonstrated right upper lobe atelectasis. After bronchoscopy, the patient could be extubated four days after surgery. She was discharged from Intensive Care Unit after 19 days. Postoperative echocardiography revealed no residual defect and no shunting across the patch. The patient could leave the hospital 25 days postoperatively in a very good condition.
3. Comments
Since the aortopulmonary window is such a rare disease, there is no standardized surgery technique for its treatment so far. Over time, the surgical repair evolved from simple ligation, division and suturing to different patch closure techniques [3]. Surgery is mostly performed on cardiopulmonary bypass [3]. Aortopulmonary window may be classified by Mori et al [4]: Type I (proximal) located just above the sinus of Valsalva, type II (distal) located in the uppermost portion of the ascending aorta and type III (total) involving the majority of the ascending aorta. In our presented case, the defect extended to the proximal aortic arch on the opposite of the supraaortic vessels. This atypical localization justifies performing surgery in deep hypothermic circulatory arrest to provide neuroprotection. Furthermore, the surgical management was complex and challenging due to of the young age and low weight of the patient. Conventionally, surgery is tried to postpone until a higher weight is attained to decrease the risk of bypass-related complications such as coagulopathy, renal dysfunction and intracranial hemorrhage and finally an increased mortality [5]. In this case, delaying the surgical procedure was not possible because of the massive left-to-right-shunt following severe pulmonary hyperperfusion with increased pulmonary artery pressure.
4. Conclusions
We accomplished a very successful surgical repair of a very complex aortopulmonary window in a low-birth-weight premature born infant. Our report supports the approach to consider surgical repair as soon as the diagnosis is established, regardless of the patient's age and weight [1].
Competing Interests
None.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
References
- Gowda D, Gajjar T, Rao JN, et al. Surgical management of aortopulmonary window: 24 years of experience and lessons learned. Interact Cardiovasc Thorac Surg 25 (2017): 302-309.
- Demir IH, Erdem A, Saritas T, et al. Diagnosis, treatment and outcomes of patients with aortopulmonary window. Balkan Med J. Jun 30 (2013): 191-196.
- Backer CL, Mavroudis C. Surgical management of aortopulmonary window: a 40-year experience. Eur J Cardiothorac Surg. May 21 (2002): 773-779.
- Mori K, Ando M, Takao A, et wl. Distal type of aortopulmonary window. Report of 4 cases. Br Heart J 40 (1978): 681-689.
- Curzon CL, Milford-Beland S, Li JS, et al. Cardiac surgery in infants with low birth weight is associated with increased mortality: analysis of the Society of Thoracic Surgeons Congenital Heart Database. J Thorac Cardiovasc Surg 135 (2008): 546-551.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 75.63%
Acceptance Rate: 75.63%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
