Cul-de-Sac Technique - Coronally Advanced Double-Pedicle Flap with/ without Grafting for Papilla Reconstruction-Case Reports
Hooshang Kashani, DMD, MS, MS1, Ryutaro Kuraji2, Jaclyn C. Chalmers, DDS3, Yvonne L. Hernandez-Kapila, DDS, PhD4*
1Private practice, San Francisco, CA; Department of Orofacial Sciences, School of Dentistry, University of California San Francisco, San Francisco, CA, USA
2Department of Periodontology, The Nippon Dental University School of Life Dentistry at Tokyo, Japan.
3Section of Periodontics, School of Dentistry, University of California Los Angeles, Los Angeles, CA, USA
4Section of Biosystems and Function, School of Dentistry, University of California Los Angeles, Los Angeles, CA, USA
*Corresponding Author: Yvonne L. Hernandez-Kapila, DDS, PhD, University of California Los Angeles School of Dentistry, 10833 Le Conte Ave., Box 951668, Los Angeles, CA 90095-1668, USA.
Received: 24 June 2025; Accepted: 03 July 2025; Published: 31 July 2025
Article Information
Citation: Hooshang Kashani, DMD, MS, MS, Ryutaro Kuraji, Jaclyn C. Cul-de-Sac Technique - Coronally Advanced Double-Pedicle Flap with/ without Grafting for Papilla Reconstruction-Case Reports. Archives of Clinical and Medical Case Reports. 9 (2025): 152-156.
View / Download Pdf Share at FacebookAbstract
Background: Regeneration of the interproximal papilla remains a challenging, unpredictable aspect of periodontal surgery. This lack of predictability could be attributed to decreased blood supply, increased distance between the underlying bone and contact point, and limited surgical access that is inherently involved with the interdental space. This two case report series proposes a novel approach, the Cul-de-Sac technique, to reestablish the papilla, either with or without connective tissue grafting.
Methods: Following non-surgical therapy, two periodontally stable patients underwent the following surgical therapy to address class II interproximal recession defects between #7 and #8. Two divergent “butt-joint” incisions were made at mesiobuccal and distobuccal line angles of adjacent teeth, extending beyond the mucogingival junction. The flap and papilla were released then advanced coronally to the contact point, creating a dead-end space beneath the papilla. Based on soft tissue thickness and the defect’s interproximal recession classification, the space beneath the papilla was filled with a harvested connective tissue graft for Patient 2; Patient 1 did not receive a graft. Simple interrupted sutures at an oblique angle were used to secure the flap in this coronal position, filling the recession area.
Results: Both Case 1 and 2 achieved favorable, esthetic results at 6 weeks and 2 weeks, respectively.
Conclusions: This “Cul-de-Sac” technique offers an additional surgical method to rebuild a recessed interdental papilla. Additional research is needed to assess the long-term results and its use with other recession defects.
Keywords
<p>Gingival recession; periodontal surgery; interproximal papilla; papilla regeneration; connective tissue graft; case reports</p>
Article Details
KEY POINTS (3 maximum)
- The “Cul-de-Sac” technique offers a new method for rebuilding the interproximal papilla, using a coronally advanced flap with or without connective tissue grafting, if indicated.
- Key aspects of the surgical technique include a proper incision design with a wide pedicle base, complete flap release for passive advancement, and atraumatic tissue handling.
- The need for additional connective tissue grafting is based upon the keratinized tissue thickness at the interproximal site and the interproximal recession defect classification (Class II and III).
Introduction
The loss of the interproximal papilla either due to periodontal disease destruction, mechanical factors, or previous periodontal treatment can present unique challenges with both functional and esthetic concerns. Gingival recession classification systems account for the loss of interproximal attachment and are based on complexity in management [1-2]. For classification of interproximal attachment loss itself, Nordland and Tarnow developed a classification system based upon the location of the papilla tip relative to the contact point and the cementoenamel junction (CEJ) [3]. A Class I recession defect refers to a papilla tip lying coronal to the interproximal extent of the CEJ, whereas in a Class II defect the papilla lies apical to the interproximal CEJ yet coronal to the most apical aspect of the facial CEJ. A Class III recession defect is when apical to all aspects of the CEJ.
While non-surgical treatment is possible with orthodontic therapy or restorative therapy, this can oftentimes be insufficient [4-5]. There are numerous well-established surgical techniques to address buccal recession, and these procedures can usually be considered predictable so long as interdental bone and soft tissue levels are favorable [6-7]. Despite many case reports introducing new techniques to reestablish the interdental papilla, it remains an unpredictable aspect of periodontal surgery [8-18]. Challenges affecting interproximal papilla regeneration include blood supply, limited surgical access, tissue fragility, and distance from the underlying bone [4,9,19]. The purpose of these case reports is to introduce a novel surgical technique to rebuild the interdental papilla, either with or without connective tissue grafting.
Materials and Methods
1.1 Surgical technique
Atraumatic handling is paramount in this technique, including flap management and anesthesia technique. Anesthesia with local infiltration and intraligamentary injections may affect plasmatic circulation to the surgical field, thus regional nerve block is recommended when possible.
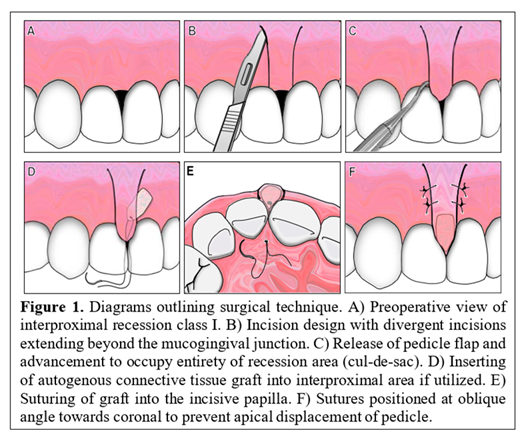
A schematic presentation of the surgical technique is shown in Figure 1A-F. Surgical informed consent was obtained. Two divergent “butt-joint” incisions are made at mesiobuccal and distobuccal line angles of adjacent teeth using #15 blade, then extended beyond the mucogingival junction (Figure 1B). It is important to make these incisions divergent to facilitate a broad base of the pedicle and ensure adequate blood supply to the double pedicle flap. Full thickness release of the coronal and papillary regions of the flap is performed by fiberotomy using either #11 blade or miniature
blades, depending on clinician preference. Release of the papilla extends to the mesiopalatal and distopalatal line angles to encompass all supracrestal fibers. Elevation of the interproximal papilla is performed using excavators (61/62 for small areas, 63/64 for larger interproximal areas), with the instrument tip in constant contact with the bone and convex portion of the instrument in contact with the flap to avoid trauma to the papilla (Figure 1C). The flap is then advanced coronally to the contact area to enable complete fill of the recession area and create a dead-end space (“cul-de-sac”) underneath the papilla. The flap must be free of tension during lip refection, with additional releasing as needed. If indicated based on keratinized tissue thickness and recession classification, a connective tissue graft is harvested at this time as seen in Case 2 (Figure 3). The graft must fit in the “cul-de- sac” interproximal space without voids and with closed, tight adaptation underneath the buccal gingiva in a symmetric fashion (Figure 1D). Immediate shrinkage of the graft after harvesting can occur due to collapsed vessels and loss of circulation, as well as secondary shrinkage during cicatrization. To compensate for this, the harvested graft should be slightly larger than the recession defect while also shaped appropriately to fit the defect shape. Using 4-0 chromic gut sutures, the connective tissue graft is sutured palatally to the incisive papilla (Figure 1E). The flap is secured passively in a coronal position with primary closure achieved by using simple interrupted sutures at oblique angles to prevent apical displacement, as pictured (Figure 1F).
1.2 Case Selection
Two patients presented to the author HK’s private practice for treatment of recession between #7 and #8, both classified as Class II interproximal recession (tip of the interdental papilla positioned at or apical to the interproximal CEJ, but coronal to the apical extent of the facial CEJ) according to Nordland and Tarnow [3]. Patient 1 (Figure 2) was a 41-year-old female with no systemic diseases or allergies. She expressed both functional concerns relating to food impaction and esthetic concerns and denied any sensitivity symptoms to hot or cold. Patient 2 (Figure 3) was a 51-year-old male with no systemic diseases and a history of orthodontic treatment. He was esthetically motivated and was advised by his orthodontist to postpone any periodontal surgery to address interproximal recessions until after completion of orthodontic therapy. Both Patient 1 and Patient 2 were periodontally stable and exhibited good or excellent oral hygiene, respectively. Patient 1 displayed periodontal probing depths of 4mm or less throughout, while Patient 2 had periodontal probing depths of 3mm or less. Neither patient displayed signs of erosion, superficial decay, or significant intrabony defects.
The need for autogenous connective tissue grafting depends on recession defect configuration and interproximal buccal gingival thickness at the recipient site. For Class I or II recession sites with greater than 2 millimeters of buccal gingiva, there is likely no need for additional grafting. For Class III defects or Class II defects with thin buccal gingiva, a connective tissue graft is required to fill in the additional interproximal space. Study models can provide helpful measurements for designing the surgery.
Initial, non-surgical periodontal therapy included plaque control, instrumentation, and oral hygiene instruction. In cases where the diseased periodontium is highly hypertrophic and inflamed, aggressive supragingival and subgingival debridement may lead to further loss of interdental papilla, thus gentle instrumentation and adequate healing time are essential.
Results
Postoperative healing was uneventful. Soft tissue fill of the interdental space was visually observed for Case 1 (Figure 2) and Case 2 (Figure 3), respectively. It is important to wait at least three months prior to probing as to not disturb the development of hemidesmosome attachment to the area. The patients did not return for additional follow-up visits beyond what is documented, we do not know whether the clinical appearance of the new papilla contour in Patient 2 persisted, in which case we could have considered minimal gingivoplasty.
Discussion
The survival of any pedicle graft with or without autogenous grafting depends on a variety of factors, including case selection and surgical technique [4,9,18,20,21]. Contraindications for this surgical technique may include presence of shallow vestibule, scar tissue from previous surgeries such as apicoectomy, poor control of systemic conditions that detrimentally affect periodontal healing, and unfavorable underlying osseous architecture. Presence of frena may also affect flap tension, though performing a frenectomy during the preliminary phase of treatment may be an option. Osseous defects in the interproximal region may affect blood supply, thus flat or positive architecture are ideal. Passive advancement of the flap is paramount for success with this technique. From a surgical standpoint, factors that could compromise the outcome of this technique include inadequate flap release at the apical and coronal portions, design of an insufficiently broad pedicle base, and unnecessary soft-tissue trauma. These would negatively influence flap circulation, leading to delayed anastomosis of the vessels and impairment of the healing process. As with all soft tissue grafting procedures, the harvested connective tissue graft can be subject to shrinkage [22-23]. For ideal esthetics, the final graft post shrinkage should have the same dimensions and contour of the interproximal space and should emulate favorable contours from the occlusal view of the recession area. Potential disadvantages of this technique include flap shrinkage leading to increased morbidity of the soft-tissue defect, papilla necrosis following surgical manipulation, or
possible esthetic concerns of the more coronally position mucogingival junction in a patient with a high smile line.
The challenges associated with interproximal papilla regeneration and lack of consensus on a superior surgical technique underscores the importance of preventing papilla loss. Numerous surgical techniques have emerged aimed at papilla preservation [3,17,24-26]. There are other proposed surgical techniques that utilize coronal advancement and connective tissue grafting, and it is important that clinicians have more than one treatment methodology to address these challenging periodontal soft-tissue defects. Advantages of this surgical technique include the incision design, with butt-joint incisions that enables primary intention closure and stability of the flap in its new position, as well as a wide pedicle base to ensure adequate plasmatic circulation.
Conclusions
The “cul-de-sac” surgical technique modifies existing soft-tissue surgery approaches to achieve esthetic reconstruction of the interproximal papilla. Additional clinical research with larger sample sizes and longitudinal re-evaluation is needed to determine its efficacy in Class I or Class III recession defects.
References
- Miller PD Jr. A classification of marginal tissue recession. Int J Periodontics Restorative Dent 5 (1985): 8-13.
- Cairo F, Nieri M, Cincinelli S, et al. The interproximal clinical attachment level to classify gingival recessions and predict root coverage outcomes: an explorative and reliability study. J Clin Periodontol 38 (2011): 661-666.
- Nordland WP, Tarnow DP. A classification system for loss of papillary height. J Periodontol 69 (1998):1124-1126.
- Blatz MB, Hürzeler MB, Strub JR. Reconstruction of the lost interproximal papilla--presentation of surgical and nonsurgical approaches. Int J Periodontics Restorative Dent 19 (1999): 395-406.
- Prato GP, Rotundo R, Cortellini P, et al. Interdental papilla management: a review and classification of the therapeutic approaches. Int J Periodontics Restorative Dent 24 (2004): 246-255.
- Cortellini P, Bissada NF. Mucogingival conditions in the natural dentition: Narrative review, case definitions, and diagnostic considerations. J Periodontol 89 (2018): S204-S213.
- Sanz M, Simion M; Working Group 3 of the European Workshop on Periodontology. Surgical techniques on periodontal plastic surgery and soft tissue regeneration: consensus report of Group 3 of the 10th European Workshop on Periodontology. J Clin Periodontol 41 (2014): S92-S97.
- Beagle JR. Surgical reconstruction of the interdental papilla: case report. Int J Periodontics Restorative Dent 12 (1992): 145-151.
- Han TJ, Takei HH. Progress in gingival papilla reconstruction. Periodontol 11 (2000): 65-68.
- Jemt T. Regeneration of gingival papillae after single-implant treatment. Int J Periodontics Restorative Dent 17 (1997): 326-333.
- Azzi R, Etienne D, Carranza F. Surgical reconstruction of the interdental papilla. Int J Periodontics Restorative Dent 18 (1998): 466-473.
- Azzi R, Etienne D, Sauvan JL, et al. Root coverage and papilla reconstruction in Class IV recession: a case report. Int J Periodontics Restorative Dent 19 (1999): 449-455.
- Tinti C, Parma-Benfenati S. The ramp mattress suture: a new suturing technique combined with a surgical procedure to obtain papillae between implants in the buccal area. Int J Periodontics Restorative Dent. 22 (2002): 63-69.
- Carnio J. Surgical reconstruction of interdental papilla using an interposed subepithelial connective tissue graft: a case report. Int J Periodontics Restorative Dent. 2004; 24 (2004): 31-37.
- McGuire MK, Scheyer ET. A randomized, double-blind, placebo-controlled study to determine the safety and efficacy of cultured and expanded autologous fibroblast injections for the treatment of interdental papillary insufficiency associated with the papilla priming procedure. J Periodontol 78 (2007): 4-17.
- Feuillet D, Keller JF, Agossa K. Interproximal Tunneling with a Customized Connective Tissue Graft: A Microsurgical Technique for Interdental Papilla Reconstruction. Int J Periodontics Restorative Dent 38 (2018): 833-839.
- Kashani H, Vora MV, Kuraji R, et al. Rebuilding the Interproximal Papilla: Description of "Tube" Technique and Two Case Reports. Clin Adv Periodontics 11 (2021): 17-21.
- Rasperini G, Tavelli L, Barootchi S, et al. Interproximal attachment gain: The challenge of periodontal regeneration. J Periodontol 92 (2021): 931-946.
- Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol 63 (1992): 995-996.
- Novaes AB Jr, Palioto DB. Experimental and clinical studies on plastic periodontal procedures. Periodontol 79 (2019): 56-80.
- Harris RJ. Double pedicle flap--predictability and aesthetics using connective tissue. Periodontol 11 (2000): 39-48.
- Scheyer ET, Sanz M, Dibart S, et al. Periodontal soft tissue non-root coverage procedures: a consensus report from the AAP Regeneration Workshop. J Periodontol 86 (2015): S73-S76.
- Zucchelli G, Tavelli L, McGuire MK, et al. Autogenous soft tissue grafting for periodontal and peri-implant plastic surgical reconstruction. J Periodontol 91 (2020): 9-16.
- Takei HH, Han TJ, Carranza FA Jr, et al. Flap technique for periodontal bone implants. Papilla preservation technique. J Periodontol 56 (1985): 204-210.
- Cortellini P, Prato GP, Tonetti MS. The modified papilla preservation technique. A new surgical approach for interproximal regenerative procedures. J Periodontol 66 (1995): 261-266.
- Cortellini P, Prato GP, Tonetti MS. The simplified papilla preservation flap. A novel surgical approach for the management of soft tissues in regenerative procedures. Int J Periodontics Restorative Dent 19 (1999): 589-599.




 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 75.63%
Acceptance Rate: 75.63%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
